Content
- The severity of COVID-19 depends on interferon
- What types of interferon are effective for coronavirus infection
- Prevention
- Treatment
- Early treatment with interferon reduces mortality and accelerates recovery, later exacerbates the disease
- Interferon type 1 + glucocorticoids
- Interferon type 1 + Janus Kinase 1/2 inhibitors
- Interferon type 2
- Interferon use in risk groups: type 2 diabetes
- Antiviral treatment that affects the interferon system
- Conclusions
- Sources
The Severity of COVID-19 Depends on Interferon
Interferon (IFN) is produced in the body in response to a viral attack and triggers all the mechanisms of antiviral defense “How interferon works”. Early production of IFN can either prevent infection or ease its course.
The SARS-CoV-2 coronavirus, which causes COVID-19, is the most vulnerable to interferon of all known coronaviruses that infect humans. SARS-CoV-2 cannot multiply if there are enough IFN molecules at the site of its penetration into the body. However, the coronavirus has different proteins to mitigate this vulnerability in every possible way:
- drown out the signal of a viral attack, according to which the synthesis of IFN begins;
- prevent the production of IFN if a sign of a viral attack did occur;
- interfere with the work of the IFN if it is produced.
That significantly delays the body’s interferon response to a coronavirus attack. The virus manages to multiply unhindered and damage almost all tissues and organs “Extrapulmonary manifestations of COVID-19“.
Late interferon response exacerbates COVID-19. The delayed interferon reaction leads to a surge in immune activity and the production of an unreasonably large number of signaling molecules – cytokines. Cytokines stimulate hyper inflammation “Cytokines storm” when cells infected with coronavirus are destroyed and healthy cells nearby. Interferon is also a cytokine, and its delayed response intensifies the cytokine storm.
Type I Interferon Protects against Hyperinflammation and Tissue Damage
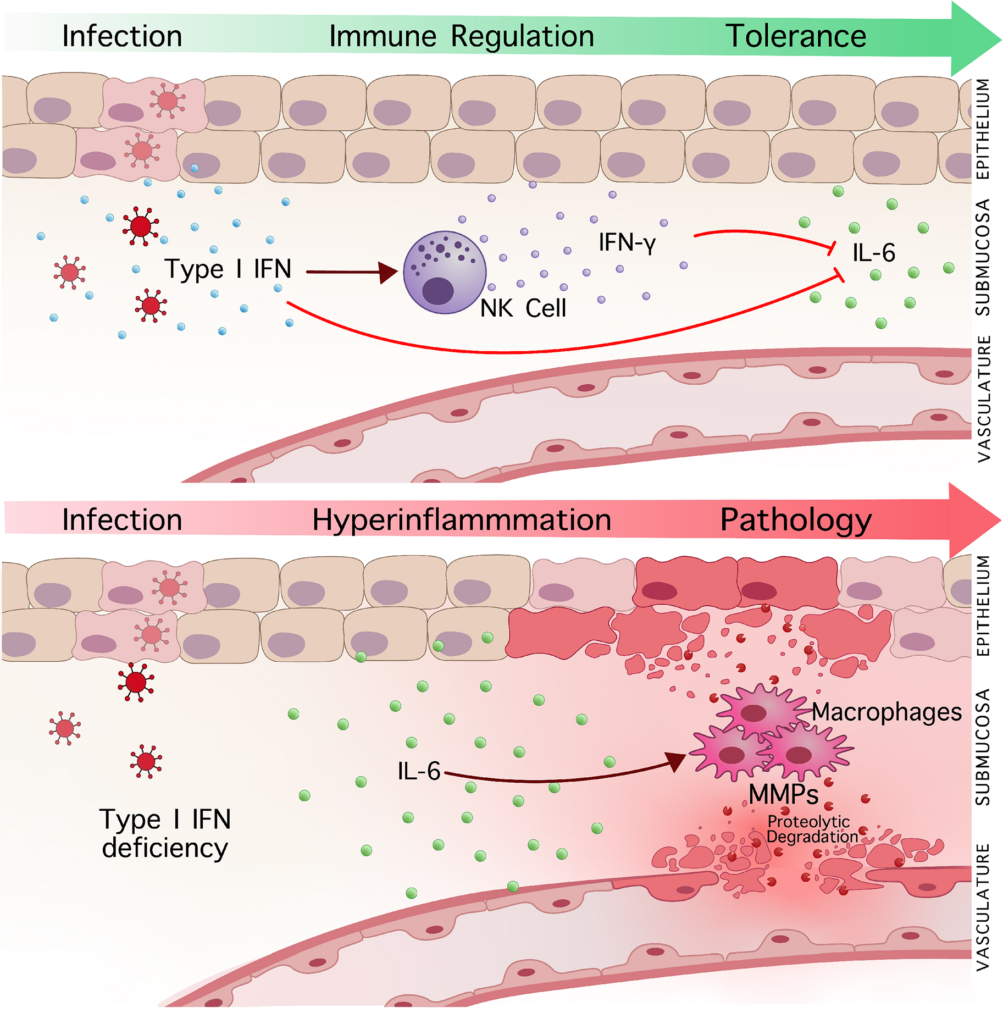
During viral infections, it is not the virus that damages tissues the most but the hyperactivation of the immune system and uncontrolled inflammation. Canadian scientists examined type I interferon’s contribution to the suppression of the virus and reduced excessive inflammatory responses, improving the outcome of the disease.
The pro-inflammatory cytokine IL-6 plays an essential role in tissue damage. Elevated IL-6 worsens severe forms of COVID-19 and influenza.
In the absence of type I interferon signaling, elevated levels of IL-6 cause hyper inflammation and tissue damage. IL-6 stimulates macrophages to produce matrix metalloproteinases (MMPs), enzymes that break down tissue structure during infection.
Type I interferon signaling inhibits increased IL-6 production and macrophage activity by inhibiting macrophage production of MMP. IFN-I promotes the activation of NK cells and the production of IFN-gamma. IFN-gamma counteracts IL-6 signaling and MMP activity, suppressing IL-6-induced inflammation and preventing tissue damage.
Macrophages and MMPs are strongly associated with tissue damage and mortality from coronavirus. Significant macrophage infiltration and MMP expression were observed in the lungs of patients with severe COVID-19.
IFN-I signaling is essential for protection against severe coronavirus. The introduction of type I interferon in the early stages prevents tissue damage, but in the later periods, it increases inflammation.
The protective mechanism of IFN is illustrated in the figure:
Image source: https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010471
Details of the study can be found in the article Type I Interferon Protects Against Hyperinflammation and Tissue Damage. The study is published in the PLOS Pathogens journal.
Diminishing Inflammation, Interferon Reduces Immune System’s Ability to Combat Secondary Infection
Type I interferons, especially interferon-β, are effectively employed in the treatment of inflammatory and autoimmune disorders, such as multiple sclerosis. Clinical observations also indicate that patients recuperating from a primary viral infection often exhibit increased susceptibility to secondary infections. This paradoxical effect can be attributed to the anti-inflammatory and immunomodulatory properties of type I interferon. Prior studies have demonstrated that interferon-β (IFN-β) suppresses the production of the potent pro-inflammatory protein interleukin-1 (IL-1).
A consortium of researchers from Austria, Germany, and Switzerland explored the mechanisms through which type I interferon modulates the severity of the inflammatory process and exerts immunosuppressive effects following a viral infection.
Type I Interferon Suppresses Synthesis and Maturation of Pro-inflammatory Protein Interleukin-1
IFN-β obstructs IL-1 production in macrophages through two distinct mechanisms:
- Initially, IFN-β inhibits the production of one of the IL-1 precursor proteins.
- Subsequently, IFN-β impedes the function of the protein responsible for IL-1 maturation.
This anti-inflammatory effect of interferon-β persists for over 6 hours.
The researchers also identified a different anti-inflammatory effect for another type I interferon – interferon-α (IFN-α). The suppressive effect of IFN-α was recorded in bone marrow-derived dendritic cells, another type of immune cell. This effect manifested only during the maturation stage of IL-1, while the production of precursor proteins remained unchanged.
Conclusion: The anti-inflammatory impact of type I interferon on IL-1 synthesis varies depending on the type of immune cells targeted.
Type I Interferon Stimulates Production of Anti-inflammatory Protein Interleukin-10
Experiments with mice demonstrated that bone marrow-derived macrophages, under the influence of IFN-1, actively produce the anti-inflammatory protein interleukin-10 (IL-10). Notably, the synthesis of IL-10, in turn, suppresses the production of the pro-inflammatory interleukin-1.
Type I Interferon Increases Susceptibility of Mice to Candidiasis
Previous studies have established that mimicking viral infections in mice diminishes their survival in candidiasis and that the pro-inflammatory protein IL-1 is crucial in combating fungal infection.
Initially, the researchers induced the production of large amounts of type I interferon in mice by introducing a safe viral infection mimic. The mice were then infected with the fungus Candida albicans, which causes candidiasis.
Post IFN-1 injections, there was a significant decrease in the survival of mice afflicted with candidiasis. The number of Candida albicans colonies in their kidneys increased, and the blood had significantly less IL-1 and its precursor protein.
Conclusion: Elevated levels of type I interferon, produced during viral infections, diminish the immune system’s ability to counter secondary infections.
Interferon-β Suppresses Production of Pro-inflammatory Protein Interleukin-1 in Human Monocytes
Human monocyte experiments, akin to those conducted on mice, exhibited the anti-inflammatory effects of IFN-β. Researchers compared monocytes from healthy volunteers with those from individuals suffering from multiple sclerosis and undergoing IFN-β treatment for symptom alleviation. Monocytes treated with interferon-β produced less IL-1.
Further details of the research are presented in the article “Type I Interferon’s Dual Effect on Immunity,” published in the journal Immunity.
How Interferon Levels Affect Disease Severity
Severe and critical forms of coronavirus infection are most often recorded in patients with disorders of the interferon system:
- insufficient production of IFN at the initial stage of the disease;
- immune abnormalities that contribute to the destruction of their own IFN;
- smokers and vapers, whose IFN system is depressed with tobacco smoke and vaping vapor “Vape, Cigarettes and Hookah Provoke Coronavirus Infection Even in Teenagers and Youngers”.
.
The link between the severity of COVID-19 and inadequate interferon production has been demonstrated in clinical studies.
One of the early studies conducted at the University of Paris and the Pasteur Institute “Severe conditions in COVID-19 are associated with the ability of SARS-CoV-2 to suppress the production of interferon in the body“. Scientists have found that in 95% of cases, low levels of IFN and suppression of the interferon-stimulated genes in patients lead to respiratory failure and acute respiratory distress syndrome requiring mechanical ventilation. The results of a series of analyzes performed at different periods of the patients’ illness revealed a clear relationship:
- patients with mild and moderate severity had a consistently high level of IFN;
- in severe patients – a short-term high level of IFN;
- in critical cases – a low level or absence of IFN.
Details of the work are published in Science magazine.
In another study, an international group of doctors from Italy, Australia, Great Britain quantitatively studied the lack of IFN in people with coronavirus infection “Dynamics of interferon-alpha in the blood of patients with COVID-19”. The level of IFN in the patients was almost 4 times lower than in people from the control group. In surviving patients, the level increased as they recovered, and in the deceased, it remained low. Details are published in the Frontiers in Immunology.
Interferon-related immune abnormalities exacerbate the course of COVID-19. Often due to comorbidities, old age, congenital genetic abnormalities, or treatment with high doses of IFN, the immune system begins to destroy the IFN molecules as if they were foreign particles “Gene mutations cause the body to attack its main antiviral proteins“. As a result, the level of IFN falls, and in case of infection with a coronavirus infection, a person gets sicker, and the blood plasma of such a recovering patient can aggravate the illness of the person to whom this plasma will be transfused.
American scientists from Yale University carried out a quantitative assessment of the number of patients with COVID-19 and immune abnormalities “Autoantibodies complicate the course of COVID-19″. They found that about 5% of hospitalized patients have antibodies against IFN, which contribute to its destruction. Details are published by Nature.
Most antibodies against interferon are found in men. They account for about 94% of such cases. That goes since the gene that regulates immune activity is located on the X chromosome “How gender affect immunity in COVID-19″. Men have one X chromosome, while women have two.
The elderly also have immune abnormalities associated with IFN. An international group of more than 150 scientists conducted a large-scale study in which it was found that approximately 4% of uninfected people over 70 years old have anomalies “Autoantibodies to interferon increase the risk of critical COVID-19 in the elderly“. These anomalies are responsible for 20% of deaths from COVID-19. Details are published in Science magazine.
Antibodies against interferon neutralize the treatment of COVID-19 with IFN drugs. This effect was demonstrated in a cell model by a joint team of scientists from the United States and France. Details of the work are published in the Journal of Experimental Medicine.
What Types of Interferon are Effective for Coronavirus Infection
There are three types of human interferon, which differ in the nuances of antiviral activityCurrent level of knowledge about human IFN. All three types are effective against COVID-19.
Type 1 interferons: alpha (α), beta (β)
- Activate the antiviral state of cells.
- They trigger the production of proteins that fight the virus at all stages of its life cycleThe role of IFN in the pagogenesis of infectious diseases.
The most studied member of this family is interferon-alpha. It is widely used in different countries of the world against the coronavirus infection “Interferon-alpha 2b for the prevention and treatment of COVID-19”.
Interferon beta is also used to treat COVID-19 but has not yet been included in national guidelines. The scientific community is still discussing the prophylactic efficacy of IFN-beta.
The rest of this type of interferon is poorly studied, and there are no approved drugs yet.
Interferon type 3: lambda (λ)
The functions of IFN-3 are similar to IFN-1 and differs is in the sphere of action. IFN-3 is produced in epithelial cells, for example, in the respiratory tract, and IFN-1 is produced by almost all cells in the body except erythrocytes and neurons. The study of type 3 interferon is in the stage of clinical trials “The role of IFN III in the control of SARS-CoV-2 in intestinal epithelial cells“ has no approved drugs yet.
Interferon type 2: gamma (γ)
- Attracts phagocyte cells to the site of infection to destroy viruses and infected cells.
- Increases the activity and survival of phagocyte cells.
- Stimulates acquired immunity to produce highly effective antiviral defense molecules “Immunological memory to the SARS-CoV-2 coronavirus: five components of the immune response“.
Clinical studies have confirmed the prophylactic efficacy of type 2 interferon against coronavirus infection.
In Cuba, for the treatment of COVID-19, type 2 interferon is used in conjunction with IFN-1.
Prevention of COVID-19
Only nasal (for the nose) forms of type 1 and type 2 interferons prevent coronavirus infection. The nose cells are the main entrance gates of the disease, and they account for the main viral attack. Nasal formulations use low doses of IFN to keep systemic exposure below the detection threshold.
Interferon type 1
The preventive efficacy of type 1 interferon against the SARS-CoV-2 coronavirus has been proven in a study by American scientists. Pretreatment of the cell culture with IFN-1 18 hours before infection reduced the multiplication rate of the coronavirus by 10,000 times on the second day of illness compared to untreated cells. Details of the study are published in the Journal of Virology.
In China, Cuba, and Russia, nasal preparations of IFN-1 are used to protect doctors of covid departments, patients’ families, international tourists, people with immunodeficiency and concomitant diseases, the elderly, pregnant women, and newborns. For more information about the preventive efficacy and the drugs used, see the review of clinical trials and extracts from the recommendations of the national health authorities “Interferon alpha-2b from coronavirus infections, influenza, and ARVI“.
Interferon type 2
Type 2 interferon nasal preparation has shown its prophylactic efficacy in a clinical study conducted in Russia. Details of the study are published in the International Journal of Biomedicine.
COVID-19 Treatment
Interferon is a highly active molecule. Therefore, treatment with systemic drugs is performed only by qualified specialists.
Early treatment with interferon reduces mortality and accelerates recovery, and later aggravates the disease
Some studies on the effectiveness of interferon in COVID-19 have revealed dependence: the timing of treatment initiation is vital – up to 5 days from the onset of symptoms.
Interferon type 1
Chinese experts studied the treatment results of 1401 patients with coronavirus infection with nebulized IFN-1 “Inhalation of interferon-α2b improves clinical outcomes of patients with COVID-19“. The best treatment results were when the drug was started 0–2 days after symptoms: less than 1% of unfavorable clinical outcomes. If the treatment was started after 6 days, then the severe or critical form of the disease was in almost 6% of cases. Details are published in the British Journal of Clinical Pharmacology.
Doctors from the UK also studied the effectiveness of nebulized IFN-1 Inhalation with interferon β-1a reduces mortality from COVID-19 and accelerates recovery. On day 28, the chances of recovery in the placebo group were 3 times lower than in the interferon group. The details of the study are published in The Lancet.
Iranian doctors investigated the safety and efficacy of subcutaneous administration of IFN-1 to patients with coronavirus infection “Systemic therapy with interferon-beta-1a reduces mortality from COVID-19 by 2 times“. The best clinical result was in patients treated with IFN:
- On day 14, 67% of patients were discharged versus 44% of patients who did not receive injections;
- 28-day mortality in the interferon group was 19%, and in the group without IFN – 43%;
- early introduction of interferon reduced the risk of death by 13 times.
Details are published in Antimicrobial Agents and Chemotherapy.
Indian scientists investigated the effectiveness of a single intramuscular injection of IFN-1 for treating patients with COVID-19 “Interferon alpha-2b is approved for the treatment of COVID-19 in India“. These people required less oxygen support than patients who received standard therapy: 56 hours versus 84. Symptoms of the disease disappeared 1 day faster in the IFN group. Details are published in the International Journal of Infectious Diseases.
Russian scientists have investigated the combined use of rectal suppositories and IFN-1 nasal gel as part of complex therapy for coronavirus infection. In the group receiving additional treatment with interferon, recovery occurred 7 days earlier than in patients receiving only standard treatment. Details are published in the Infectious Diseases.
Interferon type 1 + glucocorticoids
Chinese experts studied how effectively inhaled interferon alfa-2b is used with glucocorticoids.
A hallmark of severe COVID-19 is uncontrolled systemic inflammation due to an overactive immune system. Glucocorticoids (GCs) are anti-inflammatory drugs that doctors prescribe to reduce deaths from severe COVID-19. However, HA suppresses the interferon system, which delays eliminating the virus and has poor outcomes in various viral pneumonia.
Even in the presence of glucocorticoids, inhaled interferon effectively restores antiviral immunity. Early administration of glucocorticoids along with interferon speeds up hospital discharge, symptom relief, and virus clearance:
- Patients who received early interferon treatment (6-11 days after the onset of symptoms) and GC recovered earlier. Upon receiving GC, interferon accelerated the elimination of the virus.
- When GC and IFN were co-administered in the early stages of COVID-19, the duration of symptoms and hospital stay were shorter than when HA alone was given without IFN. However, interferon did not produce such an effect with late GC administration.
Study details – in the article “Early administration of interferon and glucocorticoids accelerates recovery from COVID-19.” The research is published in Nature journal.
Interferon Type 1 Combined With Janus Kinase 1/2 Inhibitors
The cause of the cytokine storm in COVID-19 is an inadequately strong immune response. Overactivated immune cells release potent inflammatory cytokines. Uncontrolled inflammation can lead to acute respiratory distress syndrome and multiple organ failure. In addition, the cytokine storm of COVID-19 may contribute to vascular damage and thrombosis.
High levels of inflammatory cytokines in the blood serum, observed during the COVID-19 cytokine storm, are combined with an inadequate response to IFN types I and III. SARS-CoV-2 suppresses the reaction of IFN-I and III.
Since IFN-I deficiency is associated with hyperinflammation and lower viral clearance, early treatment with interferon may prevent the virus’s rapid spread in the body and the subsequent cytokine storm.
Danish and American scientists investigated the effectiveness of Janus kinase (JAK) 1/2 inhibitors in combination with interferon alfa-2/beta to treat COVID-19.
JAK1/2 inhibitors have anti-inflammatory and immunosuppressive properties. Blocking the JAK-STAT signaling pathway suppresses the production and release of inflammatory cytokines.
Interferon and the JAK1/2 inhibitor ruxolitinib act synergistically. A Danish study confirmed the safety and efficacy of combination therapy with ruxolitinib and IFN in myelofibrosis and polycythemia vera patients. Patients quickly disappeared caused by inflammation of the clinical symptoms.
Mechanisms of joint action
Inflammation leads to the degradation of the interferon receptor, which impairs IFN signaling. However, JAK1/2 inhibitors attenuate inflammation, opening up the possibility for interferon signaling.
Interferon inhibits virus replication and shedding and also stimulates nearly all immune cells. Both interferons and the JAK1/2 inhibitor attenuate hyperinflammation, thereby reducing the likelihood of a cytokine storm.
JAK1/2 inhibitors reduce the risk of thrombosis by inhibiting inflammation-driven activation of leukocytes, platelets, endothelium, and blood coagulation.
Another factor contributing to thrombosis is extracellular traps released by neutrophils in response to inflammation. JAK1/2 inhibitors inhibit the formation of extracellular traps for neutrophils.
Interferon also reduces the risk of thrombosis. IFN-alpha-2 normalizes or significantly suppresses activated thromboinflammatory genes, substantially reduces the expression of oxidative stress genes, and activates the expression of antioxidant defense genes. Interferon-alpha-2 or interferon-beta can attenuate inflammasomes, a protein complex responsible for triggering inflammation and suppressing the formation of extracellular traps for neutrophils.
The combination of interferon-alpha-2/beta and JAK1/2 inhibitors may be superior to monotherapy in efficacy. Combination treatment of COVID-19 with ruxolitinib and interferon may shorten virus shedding and symptomatic response times, reduce the number and severity of symptoms, and reduce the risk of complications such as thrombosis and multiple organ failure.
Details of the study are placed in the article “Treatment of coronavirus: a combination of interferon and a Janus kinase 1/2 inhibitor”. The study was published in the ScienceDirect journal.
Interferon type 2
Another group of Russian specialists studied the effectiveness of IFN-2 against COVID-19. Doctors used subcutaneous injection in addition to standard therapy. The duration of hospitalization in the interferon group was 2 days less than in the group receiving only definitive treatment. Also, in the IFN group, respiratory failure did not progress, and the need for intensive care decreased. Details are published in the journal Voprosy Virologii.
French scientists have investigated the use of interferon-gamma for prolonged COVID-19. Scientists have described lingering forms of SARS-CoV-2 infection with persistent fever and poor breathing in patients receiving rituximab to treat autoimmune diseases.
Rituximab is a B-cell monoclonal antibody that depletes B cells. Patients receiving rituximab did not develop IgG antibodies to SARS-CoV-2, which slowed down the clearance of the virus.
One of the treatment methods for patients with severe coronavirus infection is the administration of convalescent plasma. However, sometimes the convalescent plasma does not have a therapeutic effect.
French scientists described a clinical case of a 68-year-old patient with lingering COVID-19, whose condition did not improve after the administration of convalescent plasma – the degree of bilateral lung damage continued to increase. The patient was prescribed therapy with interferon-gamma (IFN-γ) – 100 μg per day subcutaneously for 3 days. The introduction of IFN-γ improved the patient’s condition within a few days.
Immunotherapy with interferon-gamma improved the antiviral response by increasing the cytotoxicity of T cells and the expression of MHC molecules on the cell surface of monocytes and infected cells. IFN-γ treatment prevented the need for mechanical ventilation.
Details of the study – in the article “Interferon-gamma treats long-term coronavirus.” The study was published in the Journal of Medical Virology.
Interferon Use in Risk Groups: Type 2 Diabetes
People with type 2 diabetes are at increased risk of severe COVID-19. A common cause is a cytokine storm that causes tissue destruction and multiple organ failure. The critical cells of innate immunity – macrophages, play the leading role in developing the cytokine storm.
One of the properties of macrophages is plasticity. At the stage of development of the infection, they:
- Destroy viral particles and infected cells, and thus stimulate inflammation;
- Under the influence of cytokines, they produce additional cytokines to increase inflammation and quickly suppress the infection.
During the recovery phase from the acute phase of the disease, macrophages change their function and suppress inflammation, promoting tissue healing.
In type 2 diabetes, the SARS-CoV-2 coronavirus inhibits the plasticity of macrophages. Macrophages continue to exacerbate cytokine storms and hyper inflammation instead of suppressing inflammation and supporting organ repair. Interferon-beta restores the plasticity of macrophages. However, with coronavirus infection in people with type 2 diabetes, the level of IFN-beta is reduced to almost zero.
As a result of laboratory studies, scientists from the University of Michigan (USA) have shown that early administration of IFN-beta reduces inflammation and prevents the cytokine storm caused by macrophages in people with type 2 diabetes “Interferon prevents cytokine storm in coronavirus in diabetic patients“. Details of the study are published on the website Proceedings of the National Academy of Sciences of the USA.
Antiviral Treatment that Affects The Interferon System
Improving the effectiveness of interferon is an important strategy to combat COVID-19. The antiviral drug imidazolylethanamide pentanedioic acid increases the susceptibility of body cells to IFN molecules. The mechanism of action is based on the stimulation of the synthesis of interferon receptors on the cell surface.
Russian scientists have studied the effectiveness of the drug against COVID-19 as part of complex therapy. Research results:
| Parameter | Standard treatment + pentanedioic acid imidazolylethanamide | Standard treatment |
| Time to normalize body temperature (days) | 4,5 | 7,1 |
| Time to decrease the severity of the disease by 3 steps according to the WHO scale (days) | 10,3 | 15,0 |
| % of patients whose disease severity decreased by 3 steps on the WHO scale on day 6 | 44,4 | 10,5 |
| Time to SpO2 ≥95% (days) | 3,6 | 6,4 |
Details of the study are published in Therapy.
Conclusions
For the prevention of COVID-19, nasal forms of type 1 and type 3 interferons are used. They protect the part of the body most vulnerable to coronavirus – the nasal mucosa. The use of nasal medications is recommended for all population groups, but especially for people at risk:
- doctors of covid departments;
- families of patients;
- international tourists;
- people with immunodeficiency and concomitant diseases;
- the elderly;
- pregnant women and newborns.
For the treatment of COVID-19, nasal and systemic drugs of interferon types 1 and 3 are used. It is essential to start treatment within the first 5 days of symptom onset. Then the disease will pass more straightforward and faster. Late initiation of treatment aggravates the coronavirus infection and delays recovery.
Type I interferon operates through various mechanisms to impact inflammatory and autoimmune processes:
- On one hand, IFN-1 signaling prompts macrophages to produce fewer MMP enzymes, which cause severe tissue damage during infection. Administering type I interferon in the early stages of a viral disease aids in preserving tissue integrity. Consequently, inflammation is reduced due to the suppression of the production of pro-inflammatory proteins interleukin-1 and interleukin-6.
- Conversely, diminished inflammation enhances susceptibility to secondary infection.
Recognizing this dual effect of type I interferon is vital to improving disease prognosis while avoiding decreased survival due to secondary infections.
IFNs are highly active molecules. Therefore, treatment with systemic drugs is performed only by qualified specialists.
Sources
- Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients
- Blood Interferon-α Levels and Severity, Outcomes, and Inflammatory Profiles in Hospitalized COVID-19 Patients
- Diverse functional autoantibodies in patients with COVID-19
- Autoantibodies neutralizing type I IFNs are present in ~4% of uninfected individuals over 70 years old and account for ~20% of COVID-19 deaths
- Early nasal type I IFN immunity against SARS-CoV-2 is compromised in patients with autoantibodies against type I IFNs
- Nasopharyngeal Type-I Interferon for Immediately Available Prophylaxis Against Emerging Respiratory Viral Infections
- PROTOCOLO DE ACTUACIÓN NACIONALPARA LA COVID-19
- Type I Interferon Susceptibility Distinguishes SARS-CoV-2 from SARS-CoV
- Efficacy of Interferon Gamma in the Prevention of SARS-CoV-2 Infection (COVID-19): Results of a Prospective Controlled Trial
- Interferon-α-2b aerosol inhalation is associated with improved clinical outcomes in patients with coronavirus disease-2019
- Safety and efficacy of inhaled nebulised interferon beta-1a (SNG001) for treatment of SARS-CoV-2 infection: a randomised, double-blind, placebo-controlled, phase 2 trial
- A Randomized Clinical Trial of the Efficacy and Safety of Interferon β-1a in Treatment of Severe COVID-19
- Efficacy and safety of pegylated interferon alfa-2b in moderate COVID-19: A phase II, randomized, controlled, open-label study
- Применение препарата интерферона альфа-2b в комплексном лечении пациентов с COVID-19
- Интерферон гамма в терапии пациентов с COVID-19 среднетяжёлого течения
- Coronavirus induces diabetic macrophage-mediated inflammation via SETDB2
- Терапия пациентов с COVID-19: результаты оценки эффективности и безопасности включения препарата Ингавирин® в схему рекомендованной стандартной терапии в реальной клинической практике
- Type I interferon regulates proteolysis by macrophages to prevent immunopathology following viral infection
- Type I Interferon Inhibits Interleukin-1 Production and Inflammasome Activation