Hyperinflammation plays a vital role in the development of severe coronavirus infection. Patients develop pneumonia, gas exchange in the lungs is impaired, and acute respiratory failure appears. However, experimental treatments that block inflammatory molecules have been inconsequential.
An international group of doctors from Italy, Australia, and the UK studied inflammation profiles in hospitalized patients with COVID-19. The researchers set a goal: to examine the levels of interferon-alpha in the blood of patients with coronavirus infection, depending on the severity of the disease, the development of clinical manifestations, and the immune-inflammatory profile.
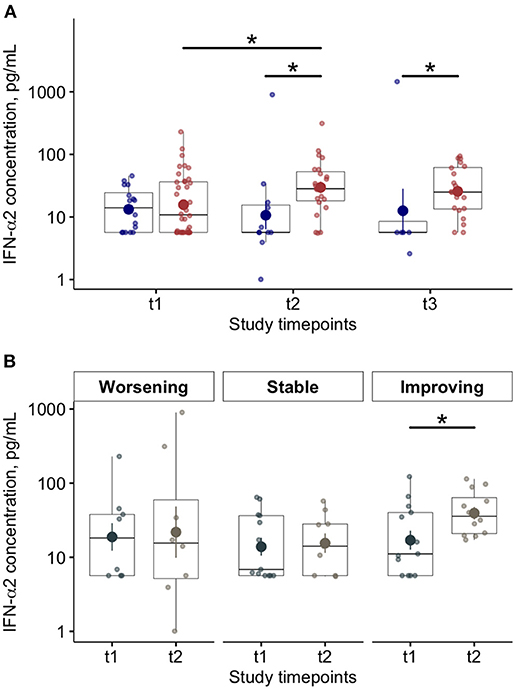
Experts have shown how the levels of pro and anti-inflammatory proteins and cells changed in patients at different periods of the disease. A severe condition in the acute phase of the disease is associated with a shortage of the pro-inflammatory molecule interferon-alpha in the body, and as the person recovers, the level of IFN-alpha in the blood increases.
Research Background
Type I interferons are a crucial component of the early defense system against viral infection. The best-studied interferon in this group is interferon-alpha.
Previous studies have shown that there is not enough IFN-alpha in the blood of patients with COVID-19. Lack of interferon contributes to severe manifestations of the disease. However, the degree of deficiency of interferon-alpha and the change in its concentration in the blood as the infection progresses have not been studied.
Understanding the immune-inflammatory mechanisms associated with the clinical manifestations of coronavirus infection can help develop new approaches to drug therapy for COVID-19.
Study Design
Doctors conducted a prospective, single-center observational study. Experts tested the hypothesis that the insufficient production of IFN-alpha in patients is one of the mechanisms that provoke a severe form of COVID-19. Researchers compared the immune-inflammatory profile in patients with COVID-19 and people without COVID-19.
The study involved 2 groups of patients:
- The first group – hospitalized people with COVID-19, respiratory failure, and oxygen saturation level less than 90%. Coronavirus infection was confirmed by PCR analysis. The group size consisted of 54 people.
- The second group is a control group, people without COVID-19 but also hospitalized with acute respiratory failure. The main reasons for hospitalization are cardiovascular disease and non-COVID-19 pneumonia. The size of the control group is 11 people.
Both groups were hospitalized between April 1, 2020, and May 31, 2020. Patients in both groups were comparable in clinical severity, age, sex, body mass index, smoking status, concomitant diseases, and the need for respiratory support. No person has previously had an immunological deficiency. No one took immunosuppressive drugs or received chemotherapy.
Research Results
The level of interferon-alpha in the blood depending on the severity of the disease and clinical outcome
Initially, in the group of patients with COVID-19, the interferon-alpha level was 3.8 times lower than in the control group. As people recovered and the severity of COVID-19 decreased, their blood levels of IFN-alpha increased significantly. In deceased patients, the level of IFN-alpha remained low throughout the disease.
Throughout the study, COVID-19 survivors had significantly higher lymphocyte levels and lower interleukin-10 (IL-10) levels than those who died from coronavirus infection.
The researchers found that clinical improvement in patients’ condition was accompanied by an increase in IFN-alpha levels and a decrease in IL-10 levels.
The figure shows the dynamics of IFN-alpha in patients with COVID-19 and the relationship between disease progression and clinical outcome. Patients who survived are marked with red dots. Blue dots are patients who have died. The interval between measurements is 7 ± 2 days.
Inflammation Profiles of Surviving and Deceased COVID-19 Patients
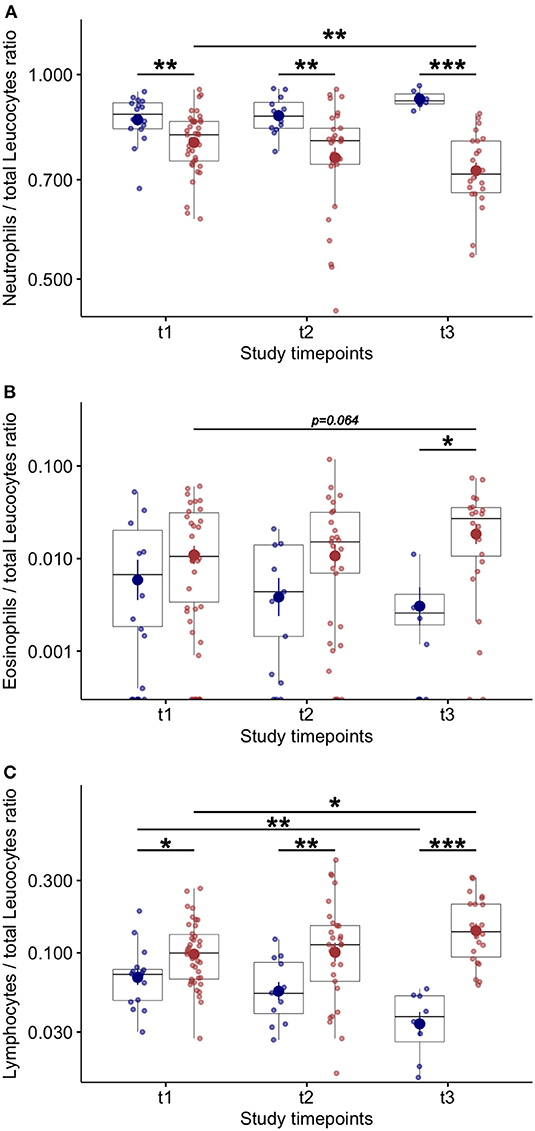
There was no difference in the number of neutrophils and eosinophils at patients’ admission to the hospital. However, the patients who died had lower lymphocyte counts, which dropped significantly over the study.
During the study, the number of eosinophils and lymphocytes increased in surviving patients.
In comparison with the survivors, the deceased had higher levels of neutrophils, C-reactive protein, procalcitonin, and IL-10 at each time point.
Researchers suggest that impaired innate immunity is associated with death from coronavirus infection.
The dynamics of the immune-inflammatory blood profile in surviving and deceased patients is shown in the figure (red dots – patients who survived, blue dots – patients who died):
Correlation Between Interferon-Alpha and Biomarkers of Immune Inflammation
Among the immunoinflammatory biomarkers tested, only IFN-gamma and IL-13 levels correlated with interferon-alpha levels. For surviving patients, the following relationship was characteristic: the higher the level of IFN-alpha, the lower the level of IL-10.
The researchers explain that IL-10 can interfere with the innate immune response and suppress the work of type I interferons. Also, IL-10 suppresses the development of an adaptive immune response. This detrimental effect further impairs antiviral responses in severe COVID-19 patients compared to controls.
Research Methods
At the beginning of the study, doctors performed clinical and immuno-inflammatory assessments of the condition of patients in both groups. Re-assessments were carried out twice more with an interval of 7 ± 2 days within a total of 21 days. Blood sampling for the study was carried out early in the morning, before the prescribed treatment.
The clinical condition of patients was assessed according to the WHO Clinical Improvement Scale:
- The need for oxygen therapy;
- The need for high-flux oxygen;
- The need for artificial ventilation.
The inflammation profile was assessed based on a multiplex immunoassay. The researchers counted inflammatory cells from blood samples and immune proteins from blood plasma samples.
A standard based on the best available evidence was used to treat patients.
Research Limitations
- All available scientific evidence, including this study, about the impaired production of IFN-I in coronavirus infection, applies only to hospitalized patients. The immunological profiles of people with coronavirus infection who do not require hospitalization remain unknown.
- Type I interferons are produced by the body very quickly, but for a short time. Therefore, collecting blood samples from patients with COVID-19 earlier from the onset of symptoms will allow a more accurate description of the role and dynamics of interferon production in coronavirus infection.
Conclusions
This study confirms the importance of interferon-alpha levels in patients with coronavirus infection. Lack of IFN-alpha leads to severe and critical forms of COVID-19, which are life-threatening.
The researchers note that baseline low IFN-alpha levels were present in all hospitalized patients regardless of clinical outcome. It proves once again that the coronavirus suppresses the production of type I interferons. However, the suppression process is not limited to the end of the acute phase of infection: longitudinal analysis has made it possible to document the restoration of immune responses in surviving patients.
Researchers suggest that the inflammatory environment of IL-10 disrupts and delays the restoration of innate immune responses.
Experts note that the results of their research can be used for drug therapy of IFN-alpha for COVID-19.
Source
https://www.frontiersin.org/articles/10.3389/fimmu.2021.648004/full