COVID-19 opens a new page in the study of viral sepsis
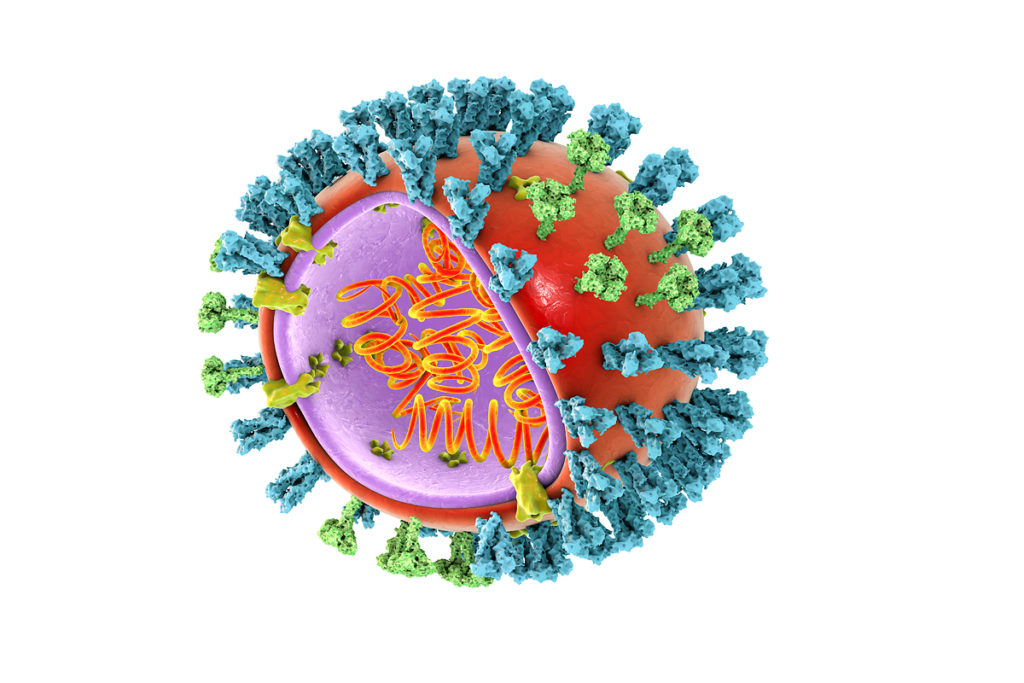
COVID-19 coronavirus infection has spread massively around the world in less than a year. High contagion, an abundance of severe complications, and insufficient knowledge have obliged WHO to declare a pandemic. To develop effective treatment and prevention tools, immune scientists comprehensively study the infection and accumulate knowledge about it.
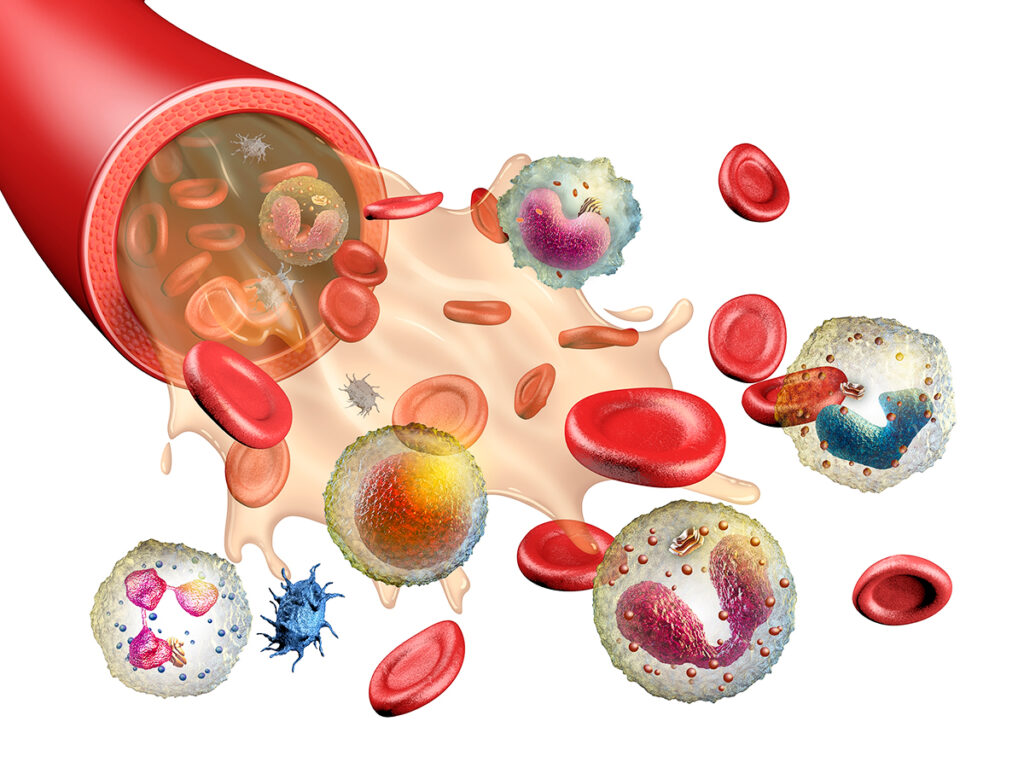
The nature of the immune response to SARS-CoV-2 is consistent with models of antiviral immunity response. Patients with severe complications have elevated levels of cytokines — proteins that regulate the strength of the immune response. Severe patients had increased thrombosis and endothelial cell death chances. This indicates damage to the blood vessels, monotremes, and the involvement of cytokines in systemic inflammation. This clinical condition, when the immune regulation is disrupted and internal organs are damaged, is called sepsis.
Despite the efforts of the scientific community and rapid progress in studying the pathogenesis of COVID-19, many complex questions remain unanswered.
Knowledge gaps in studying of COVID-19
- It is not clear what exactly causes severe complications: immune hyperactivity, cytokine storm and excess of macrophages and neutrophils in the lungs, or the inability of the body to suppress the inflammatory response due to the continued reproduction of the virus. Is pneumonia and acute respiratory distress syndrome (ARDS) associated with COVID-19 a consequence of sustained virus replication?
- How strong is the ability to tolerate increased cytokine concentrations in the systemic bloodstream, which is reduced in patients at a risk? Their blood vessels are already weakened by concomitant diseases: diabetes, hypertension, and cardiovascular diseases. What role does the increased level of cytokines play in this case: is it a protective reaction of the body or a pathological factor contributing to the disease development?
- Will monitoring patients with immune-mediated diseases help to detect abnormal cytokines? These people are treated with pro-inflammatory cytokine antagonists.
- If cytokines are neutralized, will this increase the number of complications associated with other respiratory diseases?
- Will any of the pro-inflammatory cytokine antagonists prove its effectiveness to treat severe COVID-19 patients? Previous experience shows that anti-cytokine therapy does not reduce mortality in sepsis. Why should COVID-19 be an exception?
- Will it be possible to prevent the activity of cytokines in the vascular compartment and preserve cytokine signaling in tissues that are necessary for body protection?
- Will standards for measuring cytokines be developed for comparison between cohorts? Will this method allow to detect patients advancing of a cytokine storm?
Perhaps the answers will help you better understand the immune regulation disorders and help in the treatment of different sepsis forms.
Immune response: the system of checks and balances
Under ideal conditions, the immune system provides a proportional and adequate response to the invasion of foreign particles or organisms. On the one hand, the protective response is proportional to the infectious load of the pathogen, and on the other – it is influenced by regulatory mechanisms that limit immune hyperactivity. A successful immune response to the infection is always accompanied by a certain level of inflammation and increased cytokine synthesis. It is also limited to those organs that participate in the response.
A steady level of cytokines that helps control microbes is balanced by the need to limit immune-mediated damage to the body. Excessive cytokine synthesis can lead to multiple organ failure, septic shock, and death. There are specialized regulatory cell types that have anti-inflammatory properties, as well as numerous mechanisms that mitigate the effects of cytokines. These regulatory pathways may be the result of evolution. The balance between controlling pathogens and the ability to tolerate collateral damage helps to survive the infection and develop resistance to repeated microbial invasion.
Role of cytokines in the immune system
Local cytokine synthesis begins in response to the penetration of foreign microorganisms, as well as the appearance of cancer cells or tissue damage.
Different biological activity of cytokines helps to cope with infection and restore the body faster. One of the cytokine types increases blood clotting, preventing the spread of infection. The others-stimulate the processes of suppression of foreign genetic forms, affecting T-and B-lymphocytes. Thirds — increase the permeability of the endothelium. At the same time, pro-inflammatory cytokines stimulate the growth of epithelial and connective tissue cells to accelerate the healing process and restore body integrity.
Repairing the damage, it’s activating the autoregulation mechanisms to decrease the cytokine activity. Cytokines inhibit the synthesis of themselves together with other cytokines and receptors.
In low concentrations, cytokines are needed to eliminate local damage to the body.
Increased cytokine levels and systemic inflammation
The inflammation continues to develop when the local protective reactions are not enough. As a result – a synthesis of cytokines has increased. Cytokines enter the circulation of biological fluids. The effect of cytokines is manifested on the entire body, starting a systemic inflammatory reaction and negatively affecting all organs.
High levels of cytokines affect the hypothalamus. The hypothalamus raises the body temperature to reduce the rate of propagation of pathogens. Serum cytokines stimulate the production of neutrophils and monocytes in the bone marrow, which are attracted to the epicenter of inflammation, and suppress the infection.
Cytokines change the ionic composition of the blood. There are fewer iron ions to slow down the growth of bacteria. At the same time, the level of zinc increases, normalizing the immune system, and recovering the differentiation of lymphocytes.
High levels of cytokines stimulate the hematopoietic organs to produce white blood cells that directly fight pathogens and synthesize previously died (of purulent inflammation) neutrophilic granulocytes. It also increases the production of platelets to stop bleeding and block the spread of pathogens.
Long-term systemic action of cytokines depletes the body’s reserves and disrupts the regulation of the immune system.
Abnormal cytokine levels and its manifestations
In severe cases, cytokine levels in the blood serum exceed normal thresholds and damaging various organs. The inflammation that was a defensive reaction becomes pathological.
Such hyperactivity can be associated with highly pathogenic microorganisms, certain forms of cancer, autoimmune reactions, and transplantation.
Abnormal levels of cytokines are often named as cytokine storms. It is manifested by systemic symptoms in the form of constant fever, weight loss, decreased appetite, joint and muscle pain, fatigue, and headache.
Many cytokines are associated with various forms of sepsis. It can affect vascular physiology, blood clotting, and cause concomitant tissue damage. Progressive systemic inflammation reduces vascular tone (reducing blood pressure) and develops multiple organ failure. Among them, the most prominent is respiratory failure, which also affects the heart, central nervous system, bone marrow, kidneys, spleen, and thymus. Moreover, the most vulnerable are the lungs and kidneys’ endothelium.
Abnormal levels of specific cytokines cause certain clinical manifestations. Increased levels of tumor necrosis factor-α (TNF-α) lead to the formation of disseminated blood clots, blockage of small vessels, decreased plasma volume, organ failure, septic shock, and death. High levels of interleukin-2 (IL-2) increase capillary permeability, leading to loss of liquid blood, impair oxygen transport, lead to acute respiratory failure, and damage the kidneys. Stable synthesis of interferon-g (IFN-g) and TNF-α leads to macrophage activation syndrome, which causes phagocytosis of red blood cells. All this led to the development of anemia and multiple organ failure. Abnormal levels of interleukin-6 (IL-6) cause fever, muscle pain, and headache.
Various endogenous compounds can serve as predictive indicators of cytokine storm’ secondary complications. For example, increased triglycerides can lead to pancreatitis. High levels of uric acid can cause kidney failure. Pronounced thrombocytopenia – accompanied by spontaneous intracranial hemorrhages.
Severe clinical cases – a source that allows us to study disorders of immune regulation
Complex clinical cases do not always correspond to existing pathogenesis models. New data that deny the traditional theory help the development of medical science.
The 2009 flu pandemic was caused by the H1N1 strain. Some patients had significant abnormalities in immune regulation. Coagulopathy and hemophagocytic led to deadly outcomes. Cohort analysis showed that these people had no previous immunodeficiency conditions. At the same time, genetic analysis has revealed the presence of a mutation associated with the development of hemophagocytic lymphohistiocytosis, which may have become a risk factor for death.
Another case demonstrates that sometimes a cytokine storm results in isolated damage to a single organ. In particular, the Dengue virus, which causes hemorrhagic fever, is characterized by high levels of cytokines, increased vascular permeability, and disseminated intravascular coagulation syndrome (DIC). Postmortem analysis of patients ‘ tissues revealed the presence of pulmonary edema with a relative absence of inflammation in other tissues.
Two more examples show how rapid activation of T-cells can lead to a cytokine storm. For example, some cancer treatments are aimed at enhancing the function of T-cells.
In the first case, the volunteers were intravenously injected with a drug that simultaneously activates a large number of T-cells. Within 90 minutes, a serum cytokines TNF-α, IL-2, IL-6, IL-10, IFN-g began to increase rapidly, with the appearance of symptoms of myalgia, headache, nausea, diarrhea, erythema, hypotension and vasodilation in all cases. Later, pulmonary infiltrates, lung damage, kidney failure, and DIC were developed. The decrease in the number of lymphocytes and monocytes coincided with the peak level of cytokines.
In the second case, patients with acute lymphoid leukemia were given a drug with T-cells carrying genetically modified antigen-specific receptors, which would allow them to recognize and eliminate tumor cells. After t-cell infusion, patients have been experiencing rapid development of cytokine release syndrome. Levels of IFN-g and IL-6 increased 100-1000 times, and systemic inflammation and fever further passed into macrophage activation syndrome.
These examples show how therapeutic intervention with rapid massive activation of T cells can bypass regulatory mechanisms that mitigate the effects of cytokines and have a systemic effect on the body.
Conclusions
Pathological immune responses are damaging blood vessels and internal organs which lead to a deterioration of clinical results. A better understanding of cytokine emergence at significant levels will help develop strategies for managing various forms of cytokine release syndrome.
The publication of numerous studies on COVID-19 may contribute to the identification of new underlying causes of impaired immune regulation and the development of alternative approaches. It may affect the cytokine and complement system, as well as coagulation to improve the control of various forms of sepsis.