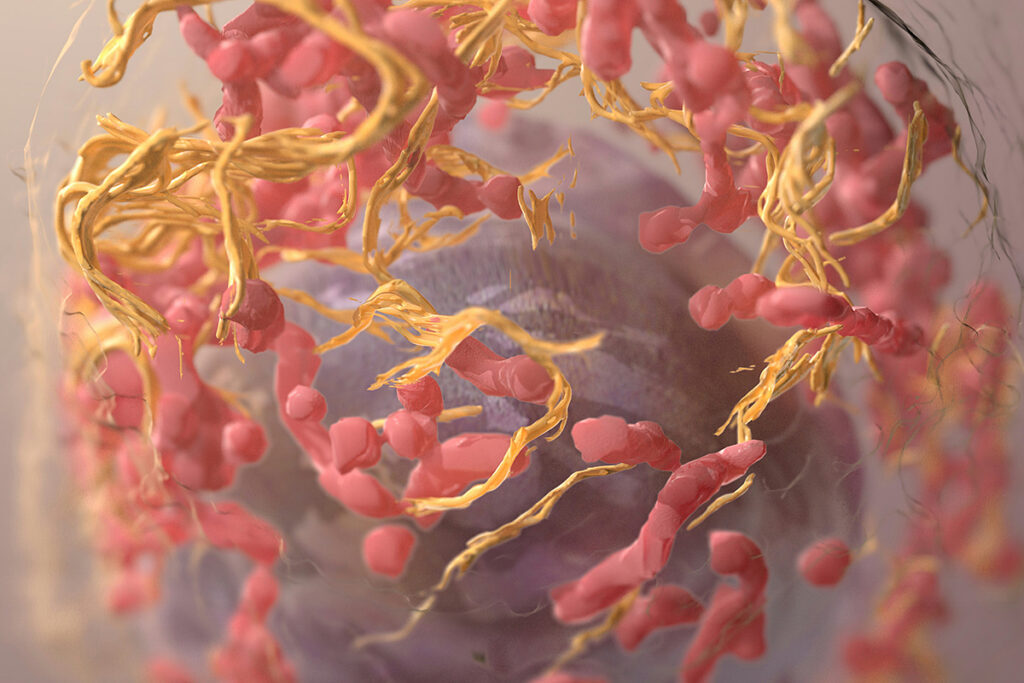
The human papillomavirus (HPV) can cause cervical cancer. Over 90% of cervical cancers (CC), including squamous intraepithelial lesion (SIL), are caused by chronic HPV infection. HPV infection disturbs the balance of the microflora of the vagina and can cause cancer of the vulva, as well as the anus and oropharynx.
Whether HPV causes cancer depends on the vaginal flora, inflammatory factors, genetics, and immune function. Chinese scientists investigated whether combination therapy with interferon α-2b and lacidophilin could improve vaginal microecology and reduce inflammation in HPV patients.
Interferon α-2b (IFNα-2b) is a protein that has antitumor, antiviral, and immunostimulatory properties. Studies confirm the antitumor properties of IFNα-2b:
- Interferon is an alternative to surgery for squamous cell neoplasia of the ocular surface. Details of the study are in the article “Interferon-Alpha-2b to Treat Ocular Surface Tumors.”
- Interferon α-2b combined with paclitaxel and 13-cis-retinoic acid is effective and safe for treating progressive and recurrent cervical cancer.
Lacidophilin – vaginal capsules based on lactic acid bacteria. Lacidophilin not only improves the microflora and acid-base balance of the vagina but also activates the immune defenses of the vagina.
Research Design
The study included 200 women aged 30-40 with HPV or low-grade squamous intraepithelial lesion (LSIL). Patients were not previously treated, were not pregnant or lactating, and had no malignant tumors or acute gynecological inflammation.
Treatment groups:
- Control group – 90 patients who injected IFNα-2b tablets into the vagina once every two days, 10 times, 3 courses.
- Investigational group – 110 patients who alternated administration of an IFNα-2b tablet on the same day and two vaginal lacidophilin capsules on the second night after IFN, 7 times, 4 courses.
In both groups, antibiotics, vaginal irrigation, bathing, and sex were prohibited during treatment. After three months, the effectiveness of treatment was evaluated.
Treatment outcomes for HPV-infected patients
After the end of treatment, in 57% of patients from the IFNα-2b and lacidophilin group, no HPV subtype was detected, and 91% of patients responded to treatment. In the IFNα-2b-only group, 48% of patients became HPV-negative, and 72% responded to treatment.
In the IFNα-2b and lacidophilin group, 90% of patients recovered the vaginal microflora. In the group, only IFNα-2b – in 66%.
Side effects assessed:
- redness and swelling of the vagina;
- tingling in the vagina;
- vaginal bleeding;
- neoplasms of the cervix or vagina.
In the IFNα-2b and lacidophilin group, side effects developed in 6, 4, 4, and 0 patients. In the IFNα-2b alone group, 4, 2, 4, and 2 patients. There was no statistical difference in the incidence of side effects: 12.73% versus 13.33%.
Conclusion
Lacidophilin vaginal capsules can significantly improve the treatment effect of IFNα-2b in HPV-infected patients. Lacidophilin restores the microflora of the vagina and suppresses inflammation.
After introduction into the cervix, lacidophilin vaginal capsules increase the number of lactic acid bacteria, which contribute to forming an anti-infective mucosal barrier, and inhibit and suppress the reproduction of harmful bacteria. Lacidophilin vaginal capsules maintain the stability of the acidic environment of the vagina and correct the disorders of the vaginal microflora.
Even though there was another drug besides interferon in the study group, the frequency of side effects did not differ from that in the control group, showing that lacidophilin increases the safety of HPV treatment.
Interferon α-2b in combination with lacidophilin can be used to prevent CC in patients with HPV infection.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary: