Diabetes mellitus (DM) is an endocrine disease characterized by a chronic increase in blood glucose levels resulting from impaired insulin secretion or action.
Because elevated blood glucose levels and diabetes suppresses the immune system, diabetic patients are more susceptible to candidiasis. Oral candidiasis is one of the most common types of fungal infection.
Candida albicans, the fungus that causes candidiasis, is part of the normal oral flora. 30-50% of people are Candida carriers. The prevalence of Candida in diabetic patients is much higher than in healthy people – 70%.
Candidiasis in diabetes is promoted by:
- accumulation of glucose in saliva;
- decreased salivation;
- easier adhesion of the fungus to the epithelium;
- decrease in microcirculation;
- reduced activity of immune cells against Candida.
In patients with type 2 diabetes mellitus (DM2), the level of interferon-gamma (IFN-γ) is increased, and the level of IL-10 is reduced:
- IL-10 is an anti-inflammatory cytokine that prevents the development of autoimmune diseases. Dysregulation of IL-10 is associated with severe immune pathologies and the risk of developing multiple autoimmune disorders. In addition, mutations in the IL-10 gene increase the risk of diabetes.
- IFN-γ is a pro-inflammatory cytokine involved in the pathogenesis of T2DM by suppressing endothelial cell function. In addition, IFN-γ is required for protection against fungal infections. However, despite elevated levels of IFN-γ in patients with T2DM, candidal infections are more common in these patients.
How are IL-10 and IFN-Γ Levels Related to Oral Candidiasis?
Iranian scientists investigated the relationship between the levels of IL-10 and IFN-γ in the blood serum of patients with type 2 diabetes and oral candidiasis. The study involved 81 patients with diabetes, and the control group consisted of 41 healthy people. In both groups, no one had factors additionally predisposing to candidiasis.
Diabetes mellitus increases the risk of candidiasis. Candidiasis was found in 51.85% of diabetic patients and 31.70% of non-diabetic patients. Among the Candida species studied, C. albicans was the most common: 45% in the diabetic group and 69% in the control group. The least common type is C. tropicalis: 4% in the diabetic group.
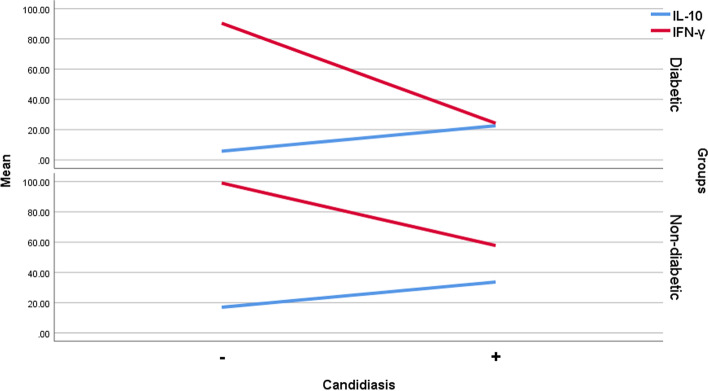
The level of IL-10 in candidiasis was significantly higher in both diabetic and control groups. In subjects without candidiasis, IL-10 levels were significantly higher in the non-diabetic group than in the diabetic group.
The level of IFN-γ in candidiasis was significantly lower in diabetics and non-diabetics.
In patients with oral candidiasis, an increase in IL-10 and a decrease in IFN-γ were observed. In the group of patients with diabetes, an increase in IL-10 increased the risk of candidiasis by 40%, and a reduction in IFN-γ increased the risk of candidiasis by 6%.
Figure. Line plot of mean IL-10 and IFN-γ values in diabetic and control groups.
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9703743/
Output
Diabetes increases the susceptibility to candidiasis. An increase in IL-10 and a decrease in IFN-γ increase the likelihood of oral candidiasis in people with diabetes by 40% and 6%, respectively.
IL-10 inhibits the antifungal activity of phagocytes and granulocytes, increasing the risk of candidiasis.
IFN-γ is needed to fight Candida albicans in the mouth and prevent the spread of infection. In response to infection of epithelial cells with Candida albicans, the production of IFN-γ increases. Low IFN-γ levels may contribute to candidiasis.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary: