Сontents
- Pregnant women and those who have recently given birth are at risk for coronavirus infection
- COVID-19 prevention measures in pregnant women
- Clinical studies of pregnant women with coronavirus infection and newborns
- The impact of coronavirus infection on pregnancy and childbirth: systematic reviews and meta-analyses
- Conclusions
- Sources
1. Pregnant women and those who have recently given birth are at risk for coronavirus infection
Center for Disease Control and Prevention informs: “To reduce the possibility of infection with coronavirus, pregnant women should be aware of the danger of the disease and pay special attention to the prevention of coronavirus infection and remove potential obstacles to comply with these measures.”
Women are most vulnerable to the coronavirus during the entire period of pregnancy and for another 42 days after delivery. During this period, they are more likely to develop severe COVID-19 than non-pregnant women. During pregnancy, changes in the body increase the risk of severe illness from all respiratory viral infections, including COVID-19. For example, an increased risk of blood clots during pregnancy may persist after delivery, and a sick woman may require hospitalization, intensive care, intubation, and mechanical ventilation.
Risks of pregnant women with COVID-19
The coronavirus increases the load on the cardiovascular system and lungs, which are already stressed during pregnancy. The course of the disease is often severe in pregnant women. Postpartum complications are more or less common in those infected with COVID-19. In rare cases, the fetus may be infected with a coronavirus. COVID-19 increases blood clotting, so when the mother is infected, it is vital to monitor the growth of the fetus.
Severe COVID-19 in pregnant women
In June 2020, the Centers for disease control and prevention (CDC, USA) released statistics:
- 8207 out of 91412 (about 9%) pregnant women with COVID-19 have a 50% increased risk of entering the intensive care unit compared to non-pregnant women of reproductive age.
- Although the death rate from COVID-19 among pregnant women is low, pregnant women are 70% more likely to need artificial ventilation.
This data only partially reflects the situation, because by June 2020, the CDC had registered 326,000 women of reproductive age with a diagnosis of COVID-19, but only 28% of them were known to be pregnant at that time or not.
According to the Swedish public health Agency, from March 19 to April 20, 2020, 53 women of reproductive age were registered in intensive care units. 13 of them are pregnant. The study found that pregnant / just-born patients with COVID-19 are 6 times more likely to end up in the intensive care unit than non-pregnant patients of reproductive age.
Pregnancy increases the risk of severe respiratory viral infections. In the United States, during the H1N1 flu epidemic in 2009, pregnant women accounted for 5% of deaths, although pregnant women made up about 1% of the population. A 2004 SARS study found that pregnant women with SARS were hospitalized more frequently and had a higher mortality rate than non-pregnant women of reproductive age.
The reason for the more severe course of viral infections in pregnant women is that the immune system should not create a significant response that can harm the baby.
Lungs and cardiovascular system of pregnant women with COVID-19
SARS-CoV-2 affects the lungs and cardiovascular system. The load on them during pregnancy is increased. When the uterus grows, there is less space for the lungs – this is the reason for shortness of breath and deterioration of lung function in pregnant women.
For the blood supply and fetus respiration, pregnant women need an additional volume of blood and oxygen. In the later stages of pregnancy – 50% more. It increases the load on the cardiovascular system.
COVID-19 also puts pressure on the heart and blood vessels. SARS-CoV-2 can affect the endothelium of the heart and blood vessels, which contains ACE2 receptors-the docking proteins of the coronavirus. These injuries cause vascular leakage and increase blood clotting. Healthy endothelial cells produce nitric oxide (NO), which regulates blood pressure, prevents inflammation, and prevents blood clots from forming. With SARS-CoV-2, endothelial function deteriorates. Blood clots can block the blood supply to vital organs.
To quickly stop bleeding after childbirth, blood clotting in pregnant women is also usually increased.
Postpartum complications with COVID-19
The New York City study of the effect of SARS-CoV-2 on pregnancy involved 675 women hospitalized for childbirth. Of these, 10% were infected with SARS-CoV-2, of which 79% had no symptoms. Postpartum complications such as fever, hypoxia, and re-hospitalization occurred in 13% of women with COVID-19 compared to 4.5% of healthy women. No women needed a ventilator, and there was no maternal mortality. None of the 71 children tested were infected with SARS-CoV‐2.
COVID-19 effect on the fetus
Viruses such as Zika virus, cytomegalovirus (CMV), and rubella can cause congenital disabilities.
A French study has shown that a fetus can be infected with COVID-19 in late pregnancy, but such cases are rare.
Virologist Caroline Coyne, who studies placental infections at the University of Pittsburgh, believes that “if the virus is a devastating pathogen that causes fetal malformations in early pregnancy, we would have obvious cases from China” in which COVID-19 started early. The staff of Science magazine got in touch with the Chinese midwives. Obstetricians confirmed that so far there have been no cases of congenital abnormalities, but warned that there is still too little data to conclude.
Rubella and CMV are usually transmitted through the blood and can reach the placenta during the first trimester before it becomes a fully formed antiviral barrier. Nevertheless, although the SARS-CoV-2 virus sometimes enters the bloodstream, it has a different transmission mechanism.
Zika virus and CMV receptors are present in large numbers on placental cells. Therefore, these viruses are dangerous for the fetus. The situation with the coronavirus is different. Scientists from the National Institute of child health and human development and Wayne State University found that placental cells rarely simultaneously Express both molecules by which SARS-CoV-2 enters the cell. These molecules are the ACE2 receptor (a docking protein of the coronavirus) and the TMPRSS-2 enzyme (an activator of the coronavirus).
COVID-19 and fetal growth
A New York City study found clots in blood vessels on the fetal side of the placenta in almost half: 14 of 29 pregnant women infected with COVID-19. In healthy pregnant women, such clots were present only in 11% of cases.
Another study, conducted by scientists from Northwestern University (USA), found significantly more damage to blood vessels and blood clots on the maternal side of the placenta in 15 of 16 infected COVID-19 women than in healthy ones.
Blood clots can limit the supply of oxygen and nutrients to the fetus. Therefore, with COVID-19 in the second half of pregnancy, it is essential to monitor the growth of the fetus.
Coronavirus during pregnancy: unsolved issues
Now the University of California, San Francisco, is collecting data for the registry of results of treatment of coronavirus in pregnancy. Data analysis will provide answers to many open questions. For example, how COVID-19 medications affect the mother and fetus, how infection affects the mother’s immune status, and whether and how to use blood clotting-reducing medications for pregnant women with COVID-19.
2. COVID-19 prevention measures in pregnant women
2.1. Recommendations of the Center for Disease Control and Prevention
Experts from the Centers for Disease Control and Prevention recommend that pregnant women, women who have recently given birth, and people who live with them or visit them must take measures to protect themselves from COVID-19.
Preventive measures:
- Limit personal communication with family members and other people who are exposed to COVID-19 or infected with the coronavirus as much as possible. The fastest coronavirus test is the presence of a sense of smell.
- Wear a mask or respirator when communicating with other people. Avoid people who don’t wear masks or ask them to wear a mask that completely covers their nose and mouth.
- Keep a distance of 1,5 meters between yourself and other people, which is about two lengths of an outstretched arm.
- Avoid crowds of people.
- Avoid poorly ventilated areas.
- Wash your hands frequently with soap and water. When soap and water are not available, use skin antiseptics with at least 60% alcohol content.
- Do not touch your eyes, nose, or mouth with unwashed hands.
- When coughing or sneezing, cover your mouth with a napkin or the inside of your elbow. After that, disinfect or wash your hands.
- Disinfect frequently used surfaces with antiseptic. For example, a mobile phone, door handles of your home, switches.
For more information about prevention measures, see the article “List of measures to reduce the risk of COVID-19 infection”.
2.2. Recommendations of the Ministry of Health of the Russian Federation on drug prevention of COVID-19 in pregnant women
For healthy individuals and individuals at risk, the Ministry of Health of the Russian Federation recommends using intranasal forms of interferon-alpha following the instructions for drug use. The drug can be in the form of a spray, drops, solution, gel, or ointment.
Pregnant women have been prescribed only intranasal drugs of recombinant interferon alpha-2b. Recombinant human interferon is produced by genetic engineering, not from blood components, so it is safe and does not risk infection with blood-borne infections. The intranasal form provides local protection against coronavirus in the nose-the entrance gate of disease. When administered intranasally, a low dose of interferon-alpha is sufficient to protect the nasal epithelium, but the dose is so tiny that it has no systemic effect.
The intranasal form of recombinant interferon alpha-2b has antiviral, anti-inflammatory, and immunomodulatory effects. The mechanism of action is based on preventing the replication of viruses that enter the body through the respiratory tract.
For more information, see the source: Temporary guidelines. Prevention, diagnosis, and treatment of new coronavirus infection (COVID-19). Version 10 (08.02.2021). Appendix 10: Recommended drug prevention regimens for COVID-19.
3. Clinical studies of pregnant women with coronavirus infection and newborns
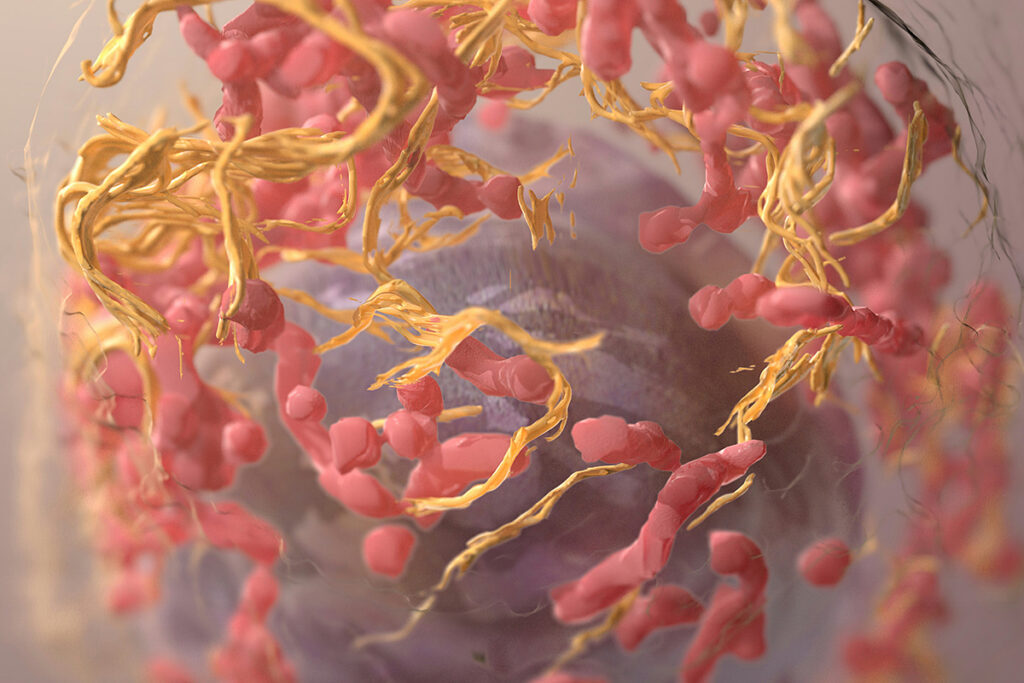
3.1. SARS-CoV-2 infects the placenta
SARS-CoV-2 is localized in syncytiotrophoblast cells – at the border of the placenta between the mother and the fetus. COVID-19 causes inflammation of the interstitial spaces of the placenta. Histological examination of the placenta showed a dense infiltration of macrophages but found no signs of vasculopathy, usually associated with preeclampsia.
In mid-March 2020, a 35-year-old woman at 22 weeks of pregnancy went to the clinic with symptoms of COVID-19. Her husband was in contact with a person with a laboratory-confirmed COVID-19 with associated symptoms. Ten days before hospitalization, the woman had a fever and cough. The symptoms have dramatically worsened over the four days before admission – high fever, malaise, dry cough, diffuse myalgia, anorexia, nausea and diarrhea.
On the morning of the treatment, the patient woke up from vaginal bleeding and abdominal pain. She did not have a fever. The breathing rate was 22 breaths per minute, and the oxygen saturation was 99% in the room air. However, the patient’s pulse is 110 beats per minute, and blood pressure is increased to 150/100 mm Hg.
Medical examination showed the presence of dark blood in the vaginal arch without dilating the cervix. A smear from the nasopharynx detected SARS-CoV-2 RNA.
The woman had a history of psoriasis with no current symptoms. Also, she had a previous pregnancy complicated by gestational hypertension. Hypertension passed with childbirth.
Hypertension is one of the signs of preeclampsia, a complication of the second half of pregnancy. During preeclampsia, vascular wall permeability increases, blood pressure increases, protein loss occurs in the urine – proteinuria, edema, and multiple organ failure occur.
The patient’s blood pressure was stable during the current pregnancy, and preeclampsia was not expected.
The patient was admitted to the maternity ward. Chest x-rays showed turbidity in the left lung. Transabdominal ultrasound revealed an active fetus weighing about 485 grams, a standard volume of amniotic fluid, and a retroplacental clot in the fundal part of the placenta. This clot indicated a possible placental abruption. Laboratory tests revealed elevated hepatic transaminases, deep thrombocytopenia, and increased protein levels in the urine – an indicator of preeclampsia. The patient also showed signs of extensive intravascular coagulation: prolonged partial thromboplastin time and decreased fibrinogen. A blood smear found atypical lymphocytes indicating viral infection and severe thrombocytopenia.
The patient was resuscitated using 4 units of cryoprecipitate, 4 pools of packed platelets, 2 grams of tranexamic acid(TXA), 5 grams of fibrinogen concentrate and 2 units of freshly frozen plasma, which reduce the coagulopathy. However, thrombocytopenia and high blood pressure remained.
The combination of hypertension, proteinuria, elevated transaminases and low platelet count confirmed the diagnosis of severe preeclampsia, which is treated by delivery.
The patient decided to terminate the pregnancy in order to reduce the risk of maternal diseases and death. Termination of pregnancy was performed under General endotracheal anesthesia by dilation and evacuation (D&E). During the operation, the retroplacental clot shown earlier by ultrasound was detected.
On the 1st day after the operation, the patient developed lymphopenia. Soon the markers of coagulation improved, and on the 3rd day after the operation, the patient was discharged for self-isolation. Blood pressure monitoring continued at home. On the 4th day, a visit to the emergency department was required to determine the dose of antihypertensive drugs. The patient agreed to a pathological examination and the transfer of tissues for research.
Hypertension and coagulopathy in pregnant women with COVID-19
Hypertensive disorders complicate 2-8% of pregnancies and rarely occur in the second trimester. Women with COVID-19 sometimes also experience hypertensive disorders. At the same time, non-pregnant patients with COVID – 19 have changed the level of liver enzymes, and impaired blood clotting-coagulopathy is observed. The same abnormalities are present in severe preeclampsia – one of the hypertensive disorders in pregnancy. Preeclampsia has increased levels of liver enzymes, reduced platelet count, proteinuria and high blood pressure.
Microbiological examination
Quantitative PCR (qRT-PCR) showed that the placenta (3 × 10 7 copies of the virus/mg) and the umbilical cord (2 × 10 3 copies of the virus/mg) were infected with SARS–CoV-2. Heart and lungs tissues of the fetus were consistent with the standards of the RNA, and the infected person was not. After the operation, the mother was also tested for SARS-CoV-2. Smears from the mouth and nose were negative, but saliva and urine were still positive. The virus from the placenta was not genetically different from SARS-CoV-2, previously found in the United States, Europe, and Australia. The SARS-CoV-2 genome from the placenta did not contain any unique amino acid substitutions compared to other sequenced SARS-CoV-2.
Serological testing
Levels of IgG and IgM antibodies to SARS-CoV-2 in the patient were among the highest among 56 patients with COVID-19 admitted to Yale hospital in new haven. The antibody titers were 1: 1600 for IgM and 1: 25,600 for IgG.
Pathology
A macroscopic examination revealed a blood clot associated with a focal placental infarction. This finding confirmed the clinical diagnosis of placental abruption. Histological examination of the placenta revealed the presence of fibrin deposits (fibrin – protein, the result of blood clotting) and inflammatory infiltrate consisting of macrophages and T-lymphocytes. It indicates inflammation of the intervillous spaces of the placenta called the intervillositis. There is no dark pigment in the interstitial space. No inflammatory cell infiltration of the vascular wall was observed in maternal vessels. The organs of the fetus are externally and microscopically unremarkable. SARS-CoV-2 is localized mainly in syncytiotrophoblastic cells of the placenta – a layer of cells that provide absorption of nutrients from the mother’s blood and produce enzymes for the introduction of chorionic villi into the uterus.
Electron microscopy
Electron microscopic analysis of the placenta showed a well-preserved ultrastructure of the placenta. Analysis of the placental region adjacent to the umbilical cord revealed SARS–CoV-2 viral particles in the cytosol of placental cells.
Fibrin deposits and macrophage infiltration in the placenta
The patient previously had gestational hypertension. That increased the risk of preeclampsia during the current pregnancy. Preeclampsia, placental abruption, and disseminated intravascular coagulopathy (DIC) are usually seen together in obstetric practice. Infection of the placenta with the SARS–CoV-2 virus shows that COVID-19 may have caused inflammation of the placenta, which led to early preeclampsia and deterioration of the mother’s condition.
Intervillusitis is characterized by fibrin deposits and the infiltration of mononuclear cells in the interstitial spaces. It is associated with a high rate of miscarriages, fetal growth retardation, and severe early preeclampsia. As a rule, intervillusitis has an autoimmune or idiopathic origin. Nevertheless, it can also be linked to infections: cytomegalovirus and malaria. Pregnant women with SARS also have fibrin deposition in the placenta.
A case of miscarriage in the second trimester of pregnancy on the background of SARS–CoV-2 was also described. The pregnant woman from the described case did not have preeclampsia, but there was an interstitial deposition of fibrin. It is not known whether COVID-19 provoked intervillusitis, but massive macrophage infiltration along with fibrin deposition was also observed in the lung tissue of patients with severe COVID-19. It increases the likelihood of immunopathology, which leads to the attraction and activation of macrophages in the tissues and causes tissue damage.
Coagulopathy in the coronavirus
Coagulopathy is observed in patients with COVID-19. It is associated with a poor prognosis. However, thrombocytopenia and fibrinogenopenia in the patient from the present study were not only associated with COVID-19. Both SARS-CoV-2 and hypertensive disorders reduce the activity of angiotensin-converting enzyme 2 (ACE2). It leads to an increase in tissue levels of angiotensin 2. Increased levels of angiotensin 2 contribute to the development of hypertensive complications, including preeclampsia in pregnant women with COVID-19. SARS-CoV-2 may reveal a predisposition to hypertensive disorders, and COVID-19 leads to placental pathology and severe patient condition.
Infection of the placenta with coronavirus
A microbiological study of the placenta showed that there are no amino acid differences in the SARS–CoV-2 genome sequenced from the placenta compared to other SARS–CoV-2 sequenced from around the world. It means that infestation through the placenta is not a unique feature of the coronavirus. Since the patient had high titers of antibodies to SARS-CoV-2, a possible mechanism of infection of the placenta is the antibody-dependent transport of substances through the cytoplasm from one pole of the cell to the other (transcytosis). The same mechanism applies to the fetal transmission of cytomegalovirus, Zika virus, and HIV.
SARS-CoV-2 is localized in placental syncytiotrophoblastic cells. It is the outer layer of multinucleated cells that cover the chorionic villi and contact the mother’s blood in the intra-dorsal space. Syncytiotrophoblasts form a cellular layer between the blood circulation of the mother and the fetus. They are involved in the transfer of protective antibodies through the placenta. Some viruses infect syncytiotrophoblasts, and the viral infection can be transmitted to fetal cells.
Acute placental infection with SARS-CoV-2 in the patient from the present study may have increased severe early preeclampsia. Identification of hypertensive disorders association with COVID-19 and diagnosis are crucial for patient care and pregnancy counselling during the coronavirus pandemic.
3.2. SARS-CoV-2 in pregnant women disrupts the placental transmission of specific antibodies
The SARS-CoV-2 infection causes more severe disease in pregnant women compared to non-pregnant women of the same age. Maternal infections disrupt the transmission of antibodies through the placenta. Scientists investigated how effectively antibodies to influenza, pertussis, and SARS-CoV-2 are transmitted through the placenta. Antibodies to influenza and whooping cough were actively transmitted. However, compared to them, the transfer of antibodies specific to SARS-CoV-2 was significantly reduced. This effect was observed only with infection in the third trimester. Impaired anti-SARS-CoV-2 antibody transfer was associated with altered anti-coronavirus glycosylation profiles. This disorder was partially eliminated by an infection-induced increase in IgG levels and increased expression of the placenta’s FCGR3A receptor. These results point to unexpected compensatory mechanisms for improving newborns’ immunity and clarifying a vaccine’s development for pregnant women and newborns.
Newborns and infants rarely get SARS-CoV-2 coronavirus. However, when infected, they can develop a severe form of COVID-19 with multisystem inflammatory syndrome, high viral load, and contagiousness. The first studies of SARS-CoV-2 among pregnant women aimed to study the possibility of vertical and placental coronavirus transmission. Later it became known that vertical and placental infections are rare.
Protection of newborns from pathogens is provided by maternal IgG antibodies transferred through the placenta. Scientists have found that antibodies to SARS-CoV-2 are carried through the placenta worse than antibodies to other diseases. The relative lack of humoral immunity transmitted from the mother creates a risk of SARS-CoV-2 infection for newborns and infants.
Although in the regions with the highest incidence, up to 16% of pregnant women test positive for SARS-CoV-2, pregnant women and newborns are excluded from the vaccine and therapeutic trials due to increased safety standards. Previous studies have shown that both newborns and pregnant women are particularly susceptible to respiratory infections, including influenza and respiratory syncytial virus. Recent data show that when infected with SARS-CoV-2, a large proportion of newborns and infants develop severe or critical diseases. Given the immature nature of the newborn immune system and the fact that developing vaccines for pregnant women and children takes longer, infants are very vulnerable during the SARS-CoV-2 coronavirus pandemic.
Placental transmission of antibodies
IgG antibodies are carried across the placenta by the neonatal Fc receptor (FcRn). To interact with the FcRn receptor, the antibody must undergo glycosylation-connect to a carbohydrate (glycan).
The transfer of placental IgG antibodies begins in the first trimester but increases exponentially during pregnancy, with most of the transfer occurring in the third trimester. Recent studies indicate a selective transfer of IgG across the placenta depends on the antibody subclass and Fc-glycan profile.
IgG1 antibodies are preferably transferred through the placenta, followed by IgG3, IgG2, and IgG4. Among IgG1 antibodies, galactosylated antibodies (combined with galactose) are preferably transferred. It may be due to stronger binding to both the placental receptor FcRn and the immune cell receptor FCGR3. That allows the most effective transfer of specific subpopulations of antibodies to newborns under the pathogen’s influence.
SARS-CoV-2 during pregnancy can disrupt the transfer of antibodies across the placenta by altering glycosylation
Recent studies have shown that SARS-CoV-2 causes changes in Fc-glycan profiles. It increases the likelihood that SARS-CoV-2 infection during pregnancy affects the quality of transmitted immunity.
According to previous studies, HIV and malaria infection in pregnant women leads to decreased placental transfer of non-specific antibodies. Impaired antibody transfer was attributed to infection-related changes in antibody glycosylation and elevated blood antibody levels (hypergammaglobulinemia) in the infected mother, leading to competition for binding placental receptor FcRn.
For most pathogens, IgG titers in the umbilical cord are higher than in maternal blood. In acute Dengue (DENV) and Zika (ZIKV) viral infections, antibody transfer coefficients of ~1.0 were observed in pregnant women, in contrast to the coefficients of 1.5 or more, commonly observed for vaccinated pathogens such as influenza and whooping cough. These lower transfer rates suggest that specific antibody glycosylation in acute infection conditions may lead to less effective placental transfer.
The researchers examined the response of humoral immunity against influenza, whooping cough, and SARS-CoV-2 in 22 pregnant women with a positive test for SARS-CoV-2 in the third trimester of pregnancy (COVID-19+) and 34 pregnant women with a negative test (COVID-19-). Antibodies targeting influenza hemagglutinin (HA) and pertussis pertactin (PTN) were effectively transferred in both groups of pregnant women. However, the transfer of SARS-CoV-2-specific IgG antibodies was significantly worse. Instead of the umbilical cord’s expected active transfer, resulting in higher titers of umbilical cord antibodies than maternal titers, reduced titers of RBD- and S-specific antibodies were present in the umbilical cord. The titers of N-specific antibodies in the umbilical cord were stable or slightly reduced.
Violation of placental transfer of antibodies to the SARS-CoV-2 coronavirus was observed only in pregnant women infected in the third trimester. Moreover, the time from infection did not significantly affect the transfer rate. In the second trimester, the placental transfer of antibodies to SARS-CoV-2 remained effective.
Increased IgG levels and closer proximity of FcRn and FCGR3A receptors compensate for low placental transfer of SARS-CoV-2 antibodies
Even though pregnant women did not have clinical hypergammaglobulinemia, COVID+ mothers had elevated IgG levels even a few weeks after infection. The total IgG titer was significantly higher in COVID+ mothers but not in their cord blood. Instead, overall IgG transfer rates were lower in COVID+ mothers. The lower the IgG level in COVID – pregnant women, the more effective the placental transfer of HA-specific antibodies was. In COVID+ pregnant women, increased IgG levels did not affect HA-IgG transfer. That suggests the presence of a compensatory mechanism during SARS-CoV-2 infection that prevents competition for antibody binding to the placental receptor FcRn observed in hypergammaglobulinemia in other infections. In contrast to the transfer of HA-specific antibodies in COVID-pregnant women, the transfer of specific antibodies to SARS-CoV-2 improved with increased IgG levels. It was probably due to a concomitant increase in SARS-CoV-2 antibodies along with an overall increase in IgG levels.
A slight increase in FCGR3A receptor expression was observed in the placenta of COVID+ pregnant women. There was no difference in the expression of the FcRn receptor. In COVID + pregnant women, these two receptors were located much closer to each other. Perhaps this is a compensatory immune mechanism specific to the third trimester of pregnancy. This mechanism can probably compensate for the violation of glycosylation in SARS-CoV-2 infection and stimulate the selection of specific antibodies that enhance the activation of natural killers that destroy infected cells to ensure the best immunity to the newborn.
Conclusions
Despite the increased susceptibility to infections of pregnant women and newborns, they are among the last to receive vaccines due to high safety requirements. Understanding gaps in the immune response in pregnant women and newborns can provide critical insights for the selection and development of therapeutics and vaccines to protect this vulnerable population effectively.
Impaired placental transfer of infection-associated antibodies was observed only in the third trimester. Understanding how antibody transfer varies by trimester will help identify the most desirable windows for vaccination to optimize protection for both mother and child.
Determining the rules for the selection and placental transfer of antibodies in the context of infection can provide vital information for the development of next-generation vaccines that provide pregnant women and newborns with stable immunity to SARS-CoV-2.
3.3. How are the levels of antibodies to coronavirus related in maternal and neonatal COVID-19
The higher the IgG level to SARS-CoV-2 in the mother’s serum, the higher the IgG level in the umbilical cord. IgM antibodies to SARS-CoV-2 were not detected in cord blood. Antibody transfer rates increase with increasing time between the onset of infection in the mother and delivery. Transfer rates are not related to the severity of the maternal disease.
The protection of newborns from infection primarily depends on the neonatal innate immune response and maternal antibodies transmitted through the placenta. The transplacental antibody transfer’s effectiveness is influenced by IgG antibody subclass, maternal infections, maternal immunodeficiency, placental pathology, and gestational age. How effectively do antibodies to the SARS-CoV-2 coronavirus penetrate the placenta? This question will help you understand whether newborns are protected from COVID-19 and develop an effective vaccination strategy for pregnant women.
Scientists at the Perelman School of Medicine at the University of Pennsylvania and the Children’s Hospital of Philadelphia (USA) investigated how the levels of antibodies to the SARS-CoV-2 coronavirus are related in a mother and a newborn. The researchers measured IgG and IgM antibodies to the receptor-binding domain (RBD) of the SARS-CoV-2 spike protein in 1,471 mother-newborn pairs and calculated the antibody transfer coefficient (infant IgG concentration divided by the mother’s IgG concentration). Results:
- 83 women (6%) had IgG or IgM antibodies to SARS-CoV-2.
- 72 infants (87%) born to seropositive women were seropositive, and 11 (13%) were seronegative.
- No seropositive children were born from 1,388 seronegative women.
- All seropositive women underwent PCR testing, except for one who declined routine obstetric testing. 44 of the 82 women tested (54%) tested positive for PCR testing.
- The majority of seropositive women (50 out of 83 [60%]) had no symptoms of COVID-19.
- Newborns were tested for SARS-CoV-2 using a PCR test between 24 and 48 hours after birth, only if the mother was PCR-positive and met the clinical criteria for infection during delivery. Among 20 of the 83 infants (24%) tested based on these criteria, none were positive.
The researchers found the following relationships between maternal and newborn antibody levels:
- The higher the IgG level to SARS-CoV-2 in the mother’s serum, the higher the IgG level in the umbilical cord.
- IgM antibodies to SARS-CoV-2 were not detected in any of the 72 seropositive infants.
- Of the 11 seropositive women who gave birth to seronegative infants, 5 women were seropositive for IgM alone. 6 remaining women had significantly lower mean IgG concentrations than 72 women with seropositive infants.
- Women with moderate or critical diseases had higher IgG and IgG concentrations, and infants born to these women had higher IgG concentrations, but these differences were not statistically significant.
- The rates of transplacental transfer of antibodies did not differ among infants born to mothers with asymptomatic and symptomatic disease.
- Transfer rates increased with increasing time between the onset of infection in the mother and delivery.
Conclusions
The researchers did not detect IgM antibodies in any cord blood serum samples, even in cases of critical maternal illness or preterm birth. It confirms that although placental and neonatal transmission of the SARS-CoV-2 coronavirus can occur, such an event is rare.
Of great concern is the possibility of postnatal infection of newborns from infectious mothers or other family members. Effective transfer of IgG antibodies to SARS-CoV-2 (transmission coefficients ≥1.0) was found in 40 of 72 children. Higher concentrations of maternal antibodies and a higher transmission rate were associated with an increased time between the onset of maternal infection and delivery.
Further studies are needed to determine whether and at what concentrations SARS-CoV-2 antibodies protect newborns and whether the transplacental kinetics of vaccine-induced antibodies are similar to naturally acquired antibodies.
4. The impact of coronavirus infection on pregnancy and childbirth: systematic reviews and meta-analyses
4.1. Canada, April 19, 2021
Scientists from the University of Montreal (Canada) published a meta-analysis of 42 studies involving 438 548 pregnant women. The researchers sought to assess the association between COVID-19 during pregnancy and adverse outcomes for the mother and fetus.
Meta-analysis result
Compared to healthy pregnant women, pregnant women with COVID-19 are:
- 82% more likely to have a preterm birth;
- 2,1 times more often a child dies in utero (stillbirth);
- 33% more likely to develop preeclampsia — high blood pressure and proteinuria. Preeclampsia can lead to premature birth, delayed fetal development, placental abruption, bleeding, thromboembolism, and strokes.
Compared to pregnant women with mild COVID-19, pregnant women with severe coronavirus infection:
- 4,2 times more likely to develop preeclampsia;
- preterm birth was 4,3 times more common;
- newborns were 1,9 times more likely to have a low body weight-less than 2500 grams;
- gestational diabetes was 2 times more likely to develop.
4.2. International Group of Scientists, September 1, 2020
An earlier meta-analysis was published by an international team of scientists from the United States, Great Britain, Switzerland, Spain, and China. We analyzed 73 studies involving 67 271 pregnant and recently delivered women with confirmed COVID-19. The scientists aimed to determine the clinical manifestations, risk factors, maternal and perinatal outcomes in pregnant and newly born women with suspected coronavirus or confirmed COVID-19.
Meta-analysis result
The most frequent clinical manifestations of coronavirus infection during pregnancy were:
- fever – in 40% of cases;
- cough – in 41% of cases.
Pregnant women with COVID-19, compared to non-pregnant women of reproductive age, who also had a confirmed diagnosis of COVID-19:
- 2.1 times more likely to be hospitalized in the intensive care unit;
- they were 2,6 times more likely to receive artificial lung ventilation;
- They were 2 times more likely to require extracorporeal membrane oxygenation (ECMO).
Concomitant factors increased the risk of developing severe COVID-19 in pregnant women:
- obesity – 2,4 times;
- chronic hypertension – 2 times;
- pre-existing diabetes – 2,1 times;
- preeclampsia – 4,2 times;
- any pre-existing maternal comorbidities – 1,8 times;
- high age – 1,8 times.
Compared to healthy pregnant women, pregnant women with COVID-19:
- 2,8 times higher maternal mortality;
- newborns were 4,9 times more likely to need intensive care.
4.3. China, April 2, 2020
One of the first systematic reviews on the impact of coronavirus disease 2019 on pregnancy was published by Chinese doctors. Experts summarized the results of 18 studies involving 114 pregnant women infected with the SARS-CoV-2 coronavirus. The researchers sought to find a relationship between COVID-19 and complications in the mother, fetus, and newborn.
System review result
According to various indications, 91,0% of women in labor with COVID-19 underwent cesarean section. Preterm birth occurred in 21,3% of cases. Low body weight was found in 5,3% of newborns. Fetal distress was present in 10,7% of cases, and asphyxia was observed in 1,2% of newborns. Stillbirth and neonatal death – in 2,4% of cases.
The scientists note that all the results were obtained based on data when pregnant women were infected with the coronavirus in the third trimester.
5. Conclusions
Studies show that pregnant women have an increased risk of severe coronavirus disease in 2019 (COVID-19). According to the Centers for Disease Prevention and Control, they are more likely than non-pregnant women to need:
- intensive care: 10,5 vs 3,9 per 1,000 cases;
- in artificial lung ventilation: 2,9 vs 1,1 per 1000 cases;
- in extracorporeal membrane oxygenation (ECMO): 0,7 vs 0,3 per 1000 cases;
- death: 1,5 vs 1,2 per 1000 cases.
To reduce the risk of severe illness and death from COVID-19, pregnant women and their family members should understand the importance of following prevention measures and seek immediate medical attention if symptoms of SARS-CoV-2 infection occur.
To minimize the risk of SARS-CoV-2 infection, pregnant women should limit unnecessary interaction with individuals who may have contracted SARS-CoV-2, including family members. When going out or interacting with others, pregnant women should wear a mask, keep a safe distance, avoid people who do not wear a mask and often disinfect their hands. In addition, pregnant women should take general measures to maintain their health and undergo routine vaccination.
6. Sources
- Characteristics of Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–June 7, 2020
- Pregnant and Recently Pregnant People
- Временные методические рекомендации. Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19). Версия 10 (08.02.2021)
- The impact of COVID-19 on pregnancy outcomes: a systematic review and meta-analysis
- Clinical manifestations, risk factors, and maternal and perinatal outcomes of coronavirus disease 2019 in pregnancy: living systematic review and meta-analysis
- Coronavirus disease 2019 (COVID-19) and pregnancy: a systematic review
- Update: Characteristics of Symptomatic Women of Reproductive Age with Laboratory-Confirmed SARS-CoV-2 Infection by Pregnancy Status — United States, January 22–October 3, 2020
- Assessment of Maternal and Neonatal Cord Blood SARS-CoV-2 Antibodies and Placental Transfer Ratios
- Compromised SARS-CoV-2-specific placental antibody transfer
- SARS–CoV-2 infection of the placenta