Age-related changes in the brain increase the risk of dementia and are accompanied by a decline in cognitive functions, including memory impairment and reduced linguistic fluency. During aging, the sense of smell deteriorates earlier than cognitive abilities. The degradation of olfaction leads to a significant loss of gray and white matter in the brain. In 2017, an international team of scientists demonstrated that even chronic sinusitis reduces gray matter volume in brain regions associated with learning and memory.
For elderly individuals, a decline in olfaction can predict the loss of gray matter in the hippocampus, a region crucial for memory. Initially, mild cognitive impairments develop, followed by Alzheimer’s disease. Olfactory dysfunction also precedes Parkinson’s disease, frontotemporal dementia, semantic dementia, corticobasal degeneration, Creutzfeldt-Jakob disease, and schizophrenia.
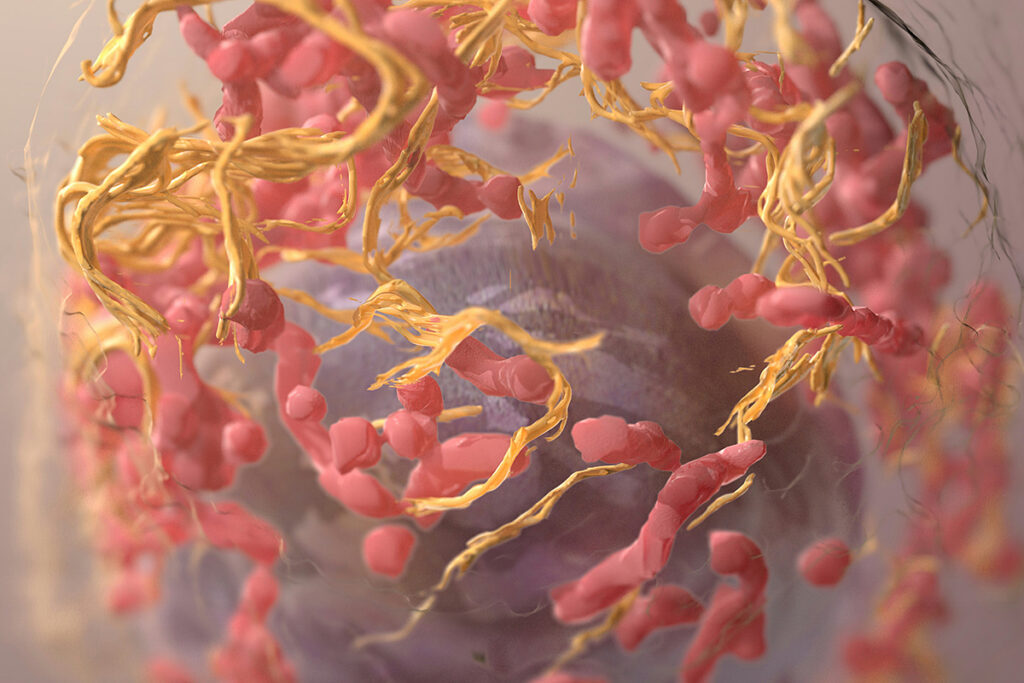
Olfaction is the only sensory system that has a direct connection to the limbic system of the brain
The limbic system is critically important for long-term and short-term memory, social-emotional interactions, and the regulation of the nervous and hormonal systems. The olfactory system has unique access to learning and memory systems. By directly affecting the nerve cells of these systems, it can prevent or reverse cognitive impairments.
Training the sense of smell stimulates neuroplasticity and improves brain structure
- In 2021, researchers from Germany and China conducted a study in which older adults were trained to recognize odors for seven months. The results were compared with a control group. MRI analysis showed that olfactory training led to an increase in the volume of cortical gray matter.
- In the same year, another group of German researchers demonstrated that daily olfactory stimulation of elderly individuals for 3-6 months reduced dementia symptoms and improved performance on the Montreal Cognitive Assessment scale.
- A similar positive effect of odor recognition training was observed in 2022 by an international team of researchers in patients with early-stage Alzheimer’s disease and individuals with mild cognitive impairments. After olfactory training, participants showed increased hippocampal cortex thickness and volume, increased entorhinal cortex thickness, and improved medial temporal lobe structure.
These studies involved rather labor-intensive odor recognition training methods, where participants practiced distinguishing dozens of aromas through multiple daily sessions, which prompted researchers from the University of California (USA) to find a less labor-intensive way to activate the olfactory system to support cognitive functions in older adults. They hypothesized that simple room aroma enrichment would achieve comparable results. In 2023, they published the results of their work.
The Study of Nighttime Aromatherapy for Cognitive Function Support
The study involved elderly individuals aged 60-85 with normal cognitive abilities and no psychiatric disorders. Participants used an automatic diffuser to scent their rooms. For 6 months, they activated the diffuser before sleep for 2 hours, dispersing one of seven aromas provided by the researchers—one aroma for each day of the week. Essential oils were used for room aromatization, including rose, orange, eucalyptus, lemon, mint, rosemary, and lavender.
Participants were randomly assigned to two groups: an experimental group that received diffuser vials with essential oils and a control group with distilled water and trace amounts of fragrance. Before and after the experiment, all participants underwent fMRI examinations to assess changes in brain structure and a series of neuropsychological assessments. Neuropsychological tests were conducted using the following methods:
- Rey Auditory Verbal Learning Test (RAVLT): evaluates learning capacity and includes five trials followed by immediate and delayed recall tests. The test assesses verbal learning, memory, recognition, attention, and recall. It is sensitive to both hippocampal integrity and cognitive dysfunction.
- Wechsler Adult Intelligence Scale (WAIS-III): A working memory test required participants to reproduce digit sequences in forward and reverse order. A test assessing planning and attention switching, featuring letter and number sequences, was also administered.
- Sniffin’ Sticks – Sensonics: A test for detecting, distinguishing, and detecting odor thresholds. This test was employed to identify olfactory abnormalities and answer whether environmental odor enrichment improves olfactory function.
In the fMRI study, researchers observed changes in major limbic pathways in the brain: the uncinate fasciculus (uncinatus fasciculus) and cingulate gyrus (gyrus cinguli). Limbic pathways are essential for episodic memory, speech, social-emotional interactions, and selecting relevant memories during information retrieval. The uncinate fasciculus plays a crucial role in learning and memory, but its functions deteriorate with age and in Alzheimer’s disease.
Nighttime Aromatherapy Enhances Cognitive Functions and Brain Structure
A significant improvement in cognitive function was observed in the experimental group, which received vials of essential oils.
In the Rey Auditory Verbal Learning Test, participants who aromatized their sleeping environment showed a 226% improvement compared to participants in the control group. The most notable enhancements were observed in word list recall, a critical test of verbal learning and memory. The graph illustrates the average difference in test results between the control group (blue column) and the experimental group (red column):
Image source: https://www.frontiersin.org/articles/10.3389/fnins.2023.1200448/full
The Wechsler Adult Intelligence Scale (WAIS-III) average score was also higher in the experimental group: 26% higher in the letter and number sequence test and 41% higher in the reverse digit reproduction test.
In several tests, no statistically significant differences were observed:
- The average score on the Wechsler Adult Intelligence Scale – forward digit reproduction test. However, a slight improvement was noted in the experimental group.
- Brief Psychiatric Rating Scale. A minor advantage was also observed in the experimental group.
- Sniffin’ Sticks – Sensonics assessment of olfactory function.
- Sleep duration. However, it increased slightly by 22 minutes in the experimental group while decreasing by 3 minutes in the control group.
The results of functional magnetic resonance imaging (fMRI) revealed a noticeable improvement in the structure of the uncinate fasciculus in the experimental group among participants aged 73-85. Participants in other age groups in the experimental group also showed structural improvement, albeit to a lesser extent.
Conclusion
Age-related changes in the brain that affect cognitive functions and increase the risk of dementia can be partially reversed or slowed down through the activation of the olfactory system. Olfaction is directly connected to the brain’s limbic system and is critically important for memory, social-emotional interactions, nervous and hormonal regulation.
Olfactory stimulation can improve cognitive abilities in people with dementia, supported by a 2022 study conducted in South Korea, where dementia patients underwent intensive olfactory training for 15 days. Significant improvements in memory, attention, and speech were observed, along with a reduction in depression. Olfactory stimulation helps enhance brain structure and function in older age.
Daily two-hour aromatherapy during sleep is sufficient to induce improvements in cognitive and neuronal functions. Such olfactory stimulation can be particularly beneficial as it does not require significant expenses or effort.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
- Overnight olfactory enrichment using an odorant diffuser improves memory and modifies the uncinate fasciculus in older adults
- Olfactory brain gray matter volume reduction in patients with chronic rhinosinusitis
- Smell training improves olfactory function and alters brain structure
- Beyond olfaction: Beneficial effects of olfactory training extend to aging-related cognitive decline
- Training with Odors Impacts Hippocampal Thickness in Patients with Mild Cognitive Impairment
- Effect of intensive olfactory training for cognitive function in patients with dementia