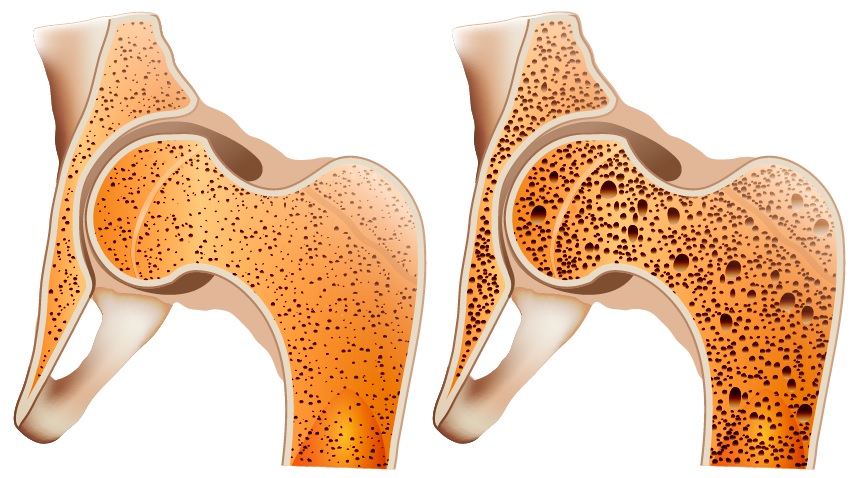
Osteoporosis is a systemic disease of the skeleton, as a result of which the volume of bone tissue in the body decreases, the density of bones decreases, and bones become brittle. Osteoporosis develops due to an imbalance between bone-destroying cells (osteoclasts) and bone-forming cells (osteoblasts). The most common fractures in osteoporosis occur in the wrists, thighs, and vertebrae.
Bone homeostasis depends on many different factors: age, postmenopausal women, inflammatory, autoimmune, and infectious diseases. One of the ways these factors affect bone health is through the immune system. The immune and skeletal systems are linked by common protein molecules and biochemical processes, particularly the interferon system.
Interferons (IFN) play an essential role in bone metabolism. However, this role is dual. In some cases, interferons stimulate the formation of bone tissue and slow down the development of osteoporosis, and in other cases contribute to the destruction of bones and exacerbate the course of the disease.
Type I interferons most often slow down the development of osteoporosis
Type I interferons are the largest group of interferons. Interferon-alpha and interferon beta (IFN-α, IFN-β) are best studied.
Interferon-alpha-2b relieved severe osteoporosis of a patient with a systemic immune disease
In 1996, Swiss doctors from the University of Bern described many years of experience treating a 33-year-old man with a rare immune disease-systemic mastocytosis. As a result of the disease, the patient developed severe osteoporosis. When the diagnosis was made, the man was found to have multiple fractures of the thoracic and lumbar vertebrae. A biopsy of the ilium showed that osteoblasts’ life expectancy and activity — the cells that form bone tissue-were reduced. Blood and urine tests indicated a severe form of osteoporosis.
For 2 years, the patient was treated with a drug of the bisphosphonate group. The treatment did not lead to a noticeable improvement. During this period, the patient suffered new vertebral fractures. However, bone mineral density (BMD) decreased more slowly than before treatment.
Swiss doctors supplemented the treatment of the man with intravenous interferon alpha-2b (IFN-a2b). For the next 2 years, the patient was treated with a combination of bisphosphonates and IFN-a2b. During the first year, the bone mineral density increased significantly, and later it remained stable.
After 2 years of treatment, the man had no new fractures, his back pain was gone, and his quality of life improved. Treatment with IFN-a2b was discontinued due to the patient’s well-being.
Interferon-β slows down the processes of bone destruction in laboratory studies
In 2015, scientists from the University of Munich (Germany) had investigated the activity of osteoclast and osteoblast genes when stimulated by interferon beta (IFN-β). The study involved 2 groups of patients. One group — people who have undergone planned hip replacement but not patients with osteoporosis. The second group — people with osteoporotic fractures and suffering from osteoporosis.
Scientists took samples of osteoblasts and osteoclasts from people from both groups. These cell cultures were then grown in a medium with interferon beta.
As a result, the scientists found that IFN-β suppresses the maturation of osteoclasts and reduces their activity. The effect was observed in both study groups. The second important conclusion is that interferon beta does not inhibit the activity of osteoblasts. Scientists suggest that the mechanism they discovered for the development of osteoporosis can be used for treatment.
In 2002, Japanese scientists at the University of Tokyo conducted a similar study on mice. Researchers have shown an important regulatory role of IFN-β in bone homeostasis. For the experiment, the scientists selected genetically modified mice that did not produce interferon beta. As a result of the study, the mice developed severe osteopenia (loss of bone mass), accompanied by increased osteoclasts’ formation. Scientists have suggested that the work may lay the molecular basis for the treatment of bone disease.
Interferon-β in clinical use has different effects on bone mineral density
In 2008, Irish doctors from St. James’ Hospital (Dublin) studied 37 patients with osteoporosis. The disease developed as a result of complications of multiple sclerosis and corticosteroid therapy.
Doctors performed immunomodulatory therapy with interferon beta-1b in all patients. As a result of the treatment, the average Z-score of the femur’s bone mineral density was 0.72, and that of the spine was 0.53. A positive BMD Z-score means that the treatment has improved the bone health of the patients. Scientists emphasize that this positive result was obtained against the background of intensive pulse therapy with corticosteroids.
Another similar study was conducted in 2010 at the University of Ataturk (Turkey). The researchers compared the BMD of patients who took IFN-β1b and patients who did not. Just as in the previous study, all subjects had osteoporosis due to complications of multiple sclerosis and pulse therapy with corticosteroids.
The researchers analyzed the T-index of BMD in both groups of patients. There was no statistically significant clinical benefit for the bones of patients from taking IFN-β1b. However, its safety has been confirmed for people with multiple sclerosis during pulse therapy with corticosteroids.
Type II Interferon in some cases stimulates the development of osteoporosis and slows down in others
The only representative of interferon type II is interferon-gamma (IFN-γ). Its functions in the body depend on the context of physiological and pathological conditions.
On the one hand, IFN-γ inhibits the formation of osteoclasts, directly affecting the progenitor cells. On the other hand, IFN-γ indirectly stimulates the formation of osteoclasts, promoting the activation of T cells and their production of proteins that stimulate the formation of osteoclasts. When the body has an estrogen deficiency or chronic inflammation, and during infection, the balance of these opposite processes shifts towards bone resorption, and osteoporosis develops.
Interferon-γ prevents bone resorption in laboratory tests
In 2000, Japanese scientists from the University of Tokyo showed that genetic defects in interferon IFN-γ lead to severe osteoporosis. The researchers found that mice with a deficiency of interferon-gamma receptors have increased bone loss due to an increased number of osteoclasts.
In 2009, an international team of scientists from the United States and South Korea investigated the mechanisms of osteoclastogenesis. An experiment on human cell culture showed that interferon-gamma prevents progenitor cells from becoming osteoclasts.
In 2011, scientists from the University of Nagasaki (Japan) continued to study the role of IFN-γ in osteoporosis. In mice, they investigated the mechanism of suppression of osteoclastogenesis by interferon-gamma. Scientists have demonstrated that IFN-γ accelerates the programmed death of osteoclasts-cells that destroy bone tissue. Also, IFN-γ neutralizes the effect of pro-inflammatory protein, which stimulates the formation of osteoclasts. Scientists suggest that through interferon-gamma, the body balances the processes of bone resorption.
Interferon-γ stimulates the development of osteoporosis in the postmenopausal period and chronic inflammation
In 2007, scientists from Emory University (USA) investigated the effect of IFN-γ on bone metabolism in mice with chronic inflammation or estrogen deficiency. Oestrogen deficiency was modeled by ovariectomy, an operation to remove the ovaries. Chronic inflammation was caused by weekly injections of lipopolysaccharide (LPS).
With estrogen deficiency and interferon-gamma deficiency, bone mass is lost more slowly than with normal levels of IFN-γ. It was found that wild-type mice lost bone mass 2 times faster than genetically modified mice with a lack of interferon-gamma. Moreover, in mice with a deficiency of the cellular receptor for IFN-γ, bone resorption did not occur after ovariectomy. Measurements of the spongy bone showed that suppression of IFN-γ after ovariectomy, although not completely, but significantly, prevents bone loss due to estrogen deficiency.
Similarly, IFN-γ affects bone resorption in chronic inflammation. Wild-type mice lost bone mass faster than IFN-γ-deficient mice. However, the difference was not as significant as in the previous case. Scientists suggest that in chronic inflammation, bone resorption is stimulated not only by interferon-gamma.
In the next experiment, the researchers showed that T-lymphocytes are vital elements of the mechanism by which interferon-gamma stimulates bone resorption. IFN-γ injections were given twice a week to two groups of mice. The first group had an excess of T-lymphocytes and the absence in the second.
T-lymphocytes are the leading producers of IFN-γ in the body. Thus, the scientists eliminated the indirect effects of IFN-γ in mice of the second group. As a result, in mice with an excess of T-lymphocytes, the mineral density of the spine bones was 3 times lower than in mice without T-lymphocytes. At the same time, osteocalcin, the marker of bone formation, did not change in any group.
Conclusions
Interferons have a complex and contradictory effect on osteoclastogenesis, bone resorption, and the development of osteoporosis.
Individual characteristics of the body, hormonal and immune background, infectious diseases, and inflammatory processes significantly affect the role of the interferon system in bone metabolism.
Sources
- Severe osteoporosis due to systemic mast cell disease: successful treatment with interferon alpha-2B
- Signaling pathway STAT1 is strongly activated by IFN-β in the pathogenesis of osteoporosis
- RANKL maintains bone homeostasis through c-Fos-dependent induction of interferon-beta
- Favorable effect of immunomodulator therapy on bone mineral density in multiple sclerosis
- The effect of interferon beta 1B on bone mineral density in multiple sclerosis patients
- T-cell-mediated regulation of osteoclastogenesis by signalling cross-talk between RANKL and IFN-γ
- Inhibition of RANK Expression and Osteoclastogenesis by TLRs and IFN-γ in Human Osteoclast Precursors
- IFN-γ directly inhibits TNF-α-induced osteoclastogenesis in vitro and in vivo and induces apoptosis mediated by Fas/Fas ligand interactions
- IFN-γ stimulates osteoclast formation and bone loss in vivo via antigen-driven T cell activation