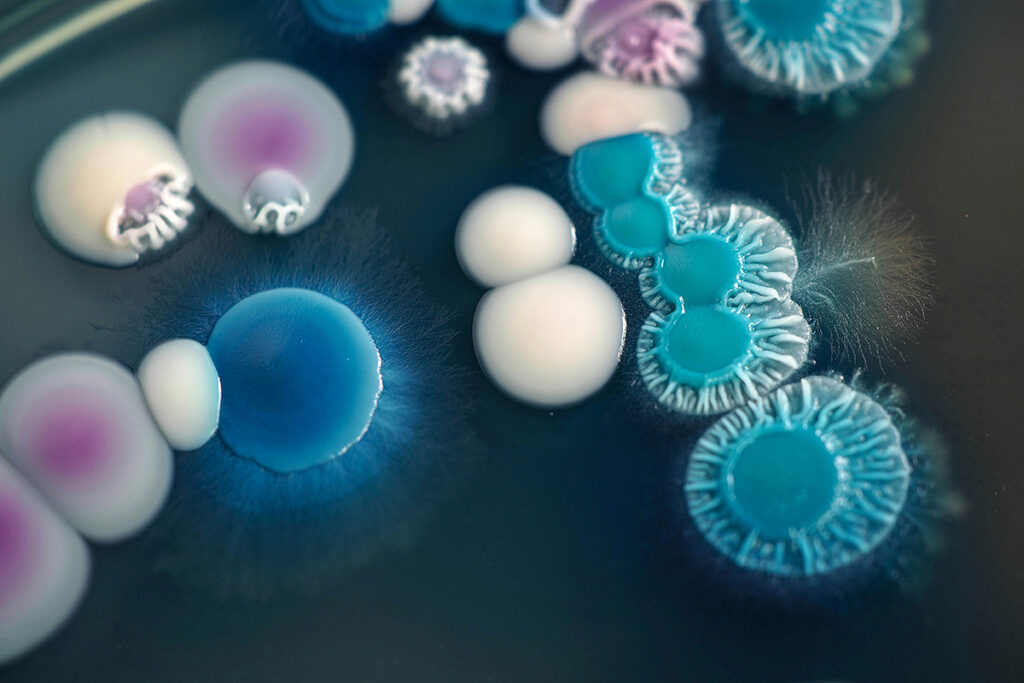
Candidiasis is the most common fungal infection caused by fungi of the genus Candida. Candidiasis can manifest both locally and systemically, affecting internal organs and tissues.
Blood infection with Candida (candidemia) is one of the nosocomial infections. Over the past decade, the prevalence of candidemia in pediatric intensive care units (ICUs) has increased dramatically. Candidemia often leads to severe illness and increases mortality among hospitalized patients.
Candida strains such as C. albicans and C. tropicalis were considered sensitive to fluconazole and amphotericin B for a long time. However, in the past few years, cases of candidiasis resistant to treatment with these drugs have been encountered in clinical practice. The reason is that long-term prophylaxis or treatment with antifungal medications has increased the number of treatment-resistant strains of Candida.
Amphotericin B, the gold standard of antifungal therapy, is used to treat systemic mycoses but can cause severe side effects because amphotericin B binds to ergosterol-rich fungal membranes but can also attack body cell membranes, destroying them. In addition, most antifungal agents only inhibit the growth of the fungus but do not destroy it.
This review collects data from laboratory and clinical studies of the antifungal activity of vitamin D3. Vitamin D3 is essential for the functioning of the immune system and plays an important protective role during inflammatory diseases. Vitamin D3 deficiency increases the risk of osteoporotic fractures, cancer, diabetes, and hypertension.
Vitamin D deficiency is common in critically ill children and ICU patients and is associated with sepsis and mortality. For example, children with serum levels of vitamin D metabolite <20 ng/mL stayed longer in the ICU. In addition, low vitamin D levels are associated with an increased incidence of acute lower respiratory infections and the need for mechanical ventilation.
D3 Kills Fungus: Lab Study
Algerian scientists have shown that vitamin D3 has antifungal activity against Candida albicans. In this study, scientists added various concentrations of vitamin D3 to test tubes containing C. albicans.
100mg/ml of vitamin D3 inhibited the growth of Candida and killed the fungus. Therefore, vitamin D3 can be used as an antifungal agent.
Vitamin D Yogurt Suppresses Fungal Growth: Clinical Study
Candida in the gastrointestinal tract increases the risk of invasive candidiasis. Prevention of Candida growth in the gastrointestinal tract with systemic antifungals reduces the prevalence of invasive fungal infections. Nevertheless, such a strategy is dangerous because of severe side effects and can lead to the emergence of drug-resistant strains of the fungus.
Chinese scientists conducted a randomized, placebo-controlled clinical trial of the antifungal activity of vitamin D. Participants in the study were 416 children aged 12 months to 5 years admitted to the intensive care unit for broad-spectrum antibiotic treatment.
Patients with candidemia were treated with intravenous amphotericin B. Patients with urinary Candida (candiduria) were treated with fluconazole.
The intervention continued for 14 days. The children were divided into two groups:
- experimental – participants received yogurt supplemented with 300 IU of vitamin D per day;
- control – participants received regular yogurt.
Research results:
- The prevalence of candiduria and candidemia was significantly lower in the vitamin D group: 26 cases versus 62.
- The mean duration of treatment with broad-spectrum antibiotics in the vitamin D group was significantly shorter than in the placebo group: 7.4 days versus 9.6 days.
- Mean ICU stay length was significantly lower in the vitamin D group: 11.8 days versus 15.2 days.
- Patient mortality was similar in both groups.
Vitamin D3 Suppresses Candida Biofilm Formation
A deficiency in vitamin D increases the risk of oral cavity candidiasis. Risk factors for candidiasis include reduced salivary flow, smoking, denture use, age, poor nutrition, malignancies, hormonal imbalances, and certain medications. In a study on HIV-infected patients, over 89% of those with candidiasis were found to have a deficiency in vitamin D. The lowest levels of vitamin D were observed in patients with both candidiasis and AIDS.
Vitamin D is essential for local immunity in the oral cavity and the production of antimicrobial peptides. A deficiency in vitamin D can lead to impaired salivary flow, creating conditions favorable for the survival of pathogenic Candida hyphae rather than harmless yeast forms. These fungal hyphae attach to the epithelium of the oral cavity and invade it, disrupting epithelial integrity.
The details of the study can be found in the article “Vitamin D Deficiency Increases the Risk of Oral Cavity Candidiasis,” published in BMC Infectious Diseases.
Long-term antifungal therapy can lead to drug resistance. Additionally, Candida forms biofilms – extracellular matrices that adhere to surfaces, protecting the fungus from the immune system and antifungal drugs.
Vitamin D3 can enhance the effectiveness of antifungal drugs. It increases the production of proteins that strengthen intercellular connections. Vitamin D exhibits antifungal activity against various Candida species, promotes the production of antimicrobial peptides, and suppresses biofilm formation by up to 88%.
The details of the study can be found in the article “Vitamin D3 Suppresses Candida Biofilm Formation,” published in Current Medical Mycology.
Conclusion
A lab study has shown that vitamin D inhibits and kills the fungus C. albicans. At the same time, preventing Candida colonization of the gastrointestinal tract reduces the risk of invasive candidiasis.
A clinical study showed that vitamin D supplementation during treatment with broad-spectrum antibiotics significantly reduced the incidence of invasive candidiasis in critically ill children. Vitamin D-fortified yogurt reduced the incidence of candiduria and candidemia.
Vitamin D supplementation effectively reduces the prevalence of fungal infections in critically ill children treated with broad-spectrum antibiotics. Taking vitamin D during antibiotic therapy will help prevent Candida infection.
Vitamin D suppresses the formation of Candida biofilms by up to 88%. It promotes the production of antimicrobial peptides, improves salivation and increases the production of proteins that strengthen intercellular bonds, preventing the survival and penetration of Candida hyphae into the epithelium. Therefore, vitamin D3 may increase the efficacy of antifungal drugs.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
References
- Vitamin D3 a new drug against Candida albicans
- Vitamin D-supplemented yogurt drink reduces Candida infections in a paediatric intensive care unit: a randomised, placebo-controlled clinical trial
- Vitamin D deficiency and oral candidiasis in patients with HIV infection: A case‒control study
- Vitamin D3: A promising antifungal and antibiofilm agent against Candida species