Oral candidiasis is a fungal disease that affects the tongue and mouth and is caused by Candida fungi. Usually, these fungi live in the mouth without causing harm, but they can cause infection under certain conditions, especially in people with weakened immune systems. Risk factors for candidiasis include impaired salivation, smoking, use of dentures, age, poor nutrition, malignant tumors, hormonal imbalances, and certain medications.
Candidiasis can appear in different forms, including plaque on the tongue and inside the cheeks, red lesions on the mucous membranes, and cracks in the corners of the mouth. Treatment includes long-term use of antifungal drugs. However, long-term treatment can lead to drug resistance and the formation of Candida biofilms.
Candidiasis is especially common in people with HIV – about 95% of patients experience this disease. Candidiasis may be one of the first signs of HIV or develop at later stages.
Vitamin D deficiency is also common among HIV patients. Vitamin D plays an essential role in oral health and immune responses. A lack of vitamin D may increase the risk of developing infections when the immune system weakens. Among these infections are tuberculosis and cytomegalovirus infections.
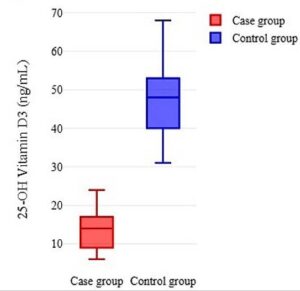
Iranian scientists investigated the relationship between vitamin D deficiency and candidiasis in patients with HIV. The study involved 206 patients with HIV: 104 – with oral candidiasis and 102 – in a control group without candidiasis. Vitamin D deficiency was defined as a 25-OH D3 level <20 ng/ml. More than 89% of patients with candidiasis were vitamin D deficient. No one in the control group was deficient.
Figure 1. Vitamin D levels in patients with candidiasis (red bar) and without (purple bar)
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10875808/
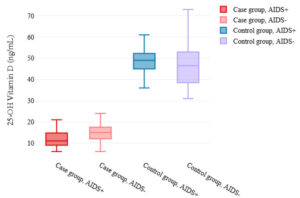
Patients with candidiasis and AIDS had significantly lower vitamin D levels than patients with candidiasis but without AIDS. In the control group, vitamin D levels did not differ between those with and without AIDS.
Figure 2. Vitamin D levels in patients with and without candidiasis, according to AIDS status
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10875808/
Conclusion
Decreased vitamin D levels and CD4 cell counts increase the risk of developing oral candidiasis in HIV-infected patients. CD4 count and viral load are critical indicators of HIV progression and response to treatment. Vitamin D deficiency is associated with decreased CD4 counts and increased viral load.
Vitamin D is involved in the regulation of innate and adaptive immunity to fight HIV. Vitamin D supplements may be beneficial for patients with HIV by increasing CD4 counts and decreasing viral load. Taking vitamin D in combination with antiretroviral therapy improves HIV control. Adequate vitamin D stimulates autophagy, inhibiting HIV replication.
Vitamin D is necessary for local immunity in the oral cavity. It helps produce antimicrobial peptides. A lack of vitamin D can lead to impaired salivation. Under these conditions, the pathogenic form of Candida survives – the hyphae form rather than the standard harmless yeast form. Fungal hyphae attach to and invade the oral epithelium, compromising its integrity. On the contrary, Vitamin D increases the production of proteins that strengthen intercellular connections. Vitamin D supplements may help HIV patients improve their oral health and prevent candidiasis.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
Vitamin D deficiency and oral candidiasis in patients with HIV infection: A case‒control study