Content
- Does a Janus kinase 1/2 inhibitor protect against cytokine storm in COVID-19
- Does interferon-alpha-2 reduce the risk of severe COVID-19
- Do statins improve the outcome of COVID-19
- Does hydroxyurea enhance the outcome of COVID-19
- Does a poor type I interferon response in older and obese people predispose to severe COVID-19?
- Do chronic inflammatory diseases increase the risk of infection and severe COVID-19
- How chronic inflammation, macrophages, and severe COVID-19 are linked
- Interferon and ACE2
- Reference
Does A Janus Kinase 1/2 Inhibitor Protect Against Cytokine Storm in COVID-19
By blocking the JAK-STAT signaling pathway, Janus kinase (JAK) 1/2 inhibitors suppress the production of inflammatory cytokines. JAK1/2 inhibitors inhibit overactivated immune cells and have an anti-inflammatory effect.
Ruxolitinib and baricitinib are JAK1/2 inhibitors. Ruxolitinib is used to treat chronic blood cancers such as myelofibrosis and polycythemia vera (MPN). Baricitinib is used to treat rheumatoid arthritis.
Treatment with ruxolitinib and baricitinib reduces inflammatory cytokines in patients with MPN and rheumatoid arthritis, respectively. The question for scientists was: do JAK1/2 inhibitors protect these patients from severe COVID-19?
The COVID-19 Treatment Guidelines do not recommend using JAK1/2 inhibitors to treat coronavirus. The reason is that ruxolitinib weakens cellular immunity, suppressing almost all immune cells. This broad immunosuppressive effect could exacerbate COVID-19.
MPN management guidelines during the COVID-19 pandemic note that MPN patients treated with JAK1/2 inhibitors are at higher risk of contracting COVID-19.
However, if a patient with MPN is affected by COVID-19, ruxolitinib may reduce the risk of developing a cytokine storm and prevent severe and critical illness. In addition, by attenuating the hyperinflammatory state in patients with MPN, ruxolitinib reduces the increased risk of thrombosis in COVID-19.
Ruxolitinib should not be discontinued in patients with MPN affected by COVID-19, as the coronavirus and associated hyperinflammatory condition may cause a withdrawal syndrome with rapid clinical deterioration and high mortality.
That confirms the clinical case of an 83-year-old female patient with myelofibrosis treated with ruxolitinib. After stopping ruxolitinib, the patient developed severe COVID-19. However, after restarting ruxolitinib, her condition immediately improved. At the same time, the addition of interferon-alpha-2 eliminated the viral infection.
Does Interferon-Alpha-2 Reduce The Risk of Severe COVID-19
Interferon-alpha-2 (IFN) has been used for decades to treat hepatitis B and C. It has also been used earlier in the treatment of HIV infection. There are many studies on the safety and efficacy of IFN in the treatment of COVID-19, either as monotherapy or in combination with other antiviral agents.
For the past 30 years, IFN-alpha-2 has been used to treat patients with MPN. Within weeks or months, IFN-alpha-2 normalizes the increased number of blood cells. The mechanisms of IFN-alpha-2 in MPN are associated with a robust increase in the activity of almost all immune cells: dendritic, NK-cells, T-cells and B-cells. Clinical experience shows that MPN patients treated with IFN-alpha-2 are less likely to develop infections, including viral ones.
Studies on the safety and efficacy of interferon in COVID-19 have shown that early treatment with interferon reduces mortality and speeds up recovery, but late treatment may exacerbate the disease.
Interferon administration early in COVID-19 may reduce the need for hospitalization. In addition, early treatment with interferon may reduce the risk of long-term consequences of COVID-19, including mental illness, chronic pulmonary fibrosis, chronic heart failure, or chronic kidney disease.
Do Statins Improve The Outcome of COVID-19
Statins are cholesterol-lowering drugs. In addition, they have anti-inflammatory and antithrombotic properties.
Statins block inflammatory signals and may mitigate the cytokine storm in COVID-19. Statins can also inhibit SARS-CoV-2 entry into the cell by activating the ACE2 and CD147 receptors and the cell membrane.
Statins may reduce the risk of thrombosis by increasing fibrinolytic and anticoagulant activity in the vessel wall. In addition, statins suppress the expression of clotting factor III by monocytes and macrophages.
Statins may counteract the thrombogenic state associated with COVID-19 by interfering with viral entry into cells and inhibiting the thrombogenic activity of blood cells and endothelial cells, as well as enhancing the anticoagulant and fibrinolytic properties of the inflamed endothelium.
Statins enhance the effectiveness of IFN and JAK1/2 inhibition with ruxolitinib. It opens up the possibility for further research into the treatment of COVID-19 with a combination of these drugs.
Does Hydroxyurea Enhance The Outcome Of COVID-19
Hydroxyurea is an antitumor and antiviral drug that has been used for decades to treat hematological, oncological and infectious diseases. Today, hydroxyurea is primarily used to treat MPN and sickle cell anemia (SCA).
Hydroxyurea inhibits DNA synthesis and reduces the number of tumor cells within a few days. In addition, hydroxyurea reduces elevated levels of inflammatory cytokines in SCA, an inflammatory and thrombotic disease similar to MPN and COVID-19. With all these diseases, leukocytes, platelets and endothelial cells are activated, which leads to thrombosis.
Like COVID-19, SCA is a hyperinflammatory thrombogenic disease that exacerbates the sickle cell crisis. A sickle cell crisis occurs when sickle-shaped red blood cells stick together and block the small blood vessels that carry blood to organs, muscles, and bones. In SCA, the levels of circulating inflammatory cytokines TNF-α, IL-8, IL-1β, and IL-6 are markedly elevated. Hydroxyurea reduces the level of inflammatory cytokines and the risk of thrombosis, including sickle cell crisis.
Previously, hydroxyurea was used as an antiviral drug. A laboratory study on HIV-infected lymphocytes showed that hydroxyurea inhibits viral DNA synthesis and increases the antiviral activity of didanosine. In combination with didanosine, Hydroxyurea induces potent and sustained viral suppression in patients with HIV infection.
As with HIV infection, hydroxyurea can also suppress SARS-CoV-2. Hydroxyurea reduces immune system hyperactivation, prevents CD8 T cell and CD4 T cell depletion, and avert cytokine storm in COVID-19.
Does A Weak Type I Interferon Response in Older and Obese People Predispose to Severe COVID-19
Weak type I IFN responses are associated with more extended viral clearance and severe hyperinflammation. Early treatment with interferon may hinder the progression of COVID-19 by suppressing viral replication and immune mechanisms that cause subsequent hyperinflammation.
The elderly and obese patients are at higher risk of severe COVID-19. Also, these people have an impaired interferon response. Thus, the elderly and obese patients may benefit from early treatment with interferon.
Do Chronic Inflammatory Diseases Increase The Risk of Infection and Severe COVID-19
Not only the elderly and obese but also patients with chronic inflammatory diseases are at an increased risk of developing severe COVID-19. These diseases include rheumatoid arthritis, inflammatory bowel disease, cardiovascular disease, type II diabetes mellitus, hematologic and non-hematologic cancers.
A possible mechanism for morbidity and mortality during COVID-19 is that prior inflammation implies an increased risk of rapidly developing a life-threatening cytokine storm.
Cytokine inhibitors may protect patients from severe COVID-19. A recent study showed a low prevalence of SARS-CoV-2 seroconversion in patients with inflammatory bowel disease treated with cytokine inhibitors. It means that treatment with cytokine inhibitors may at least partially protect against SARS-CoV-2 infection.
How Chronic Inflammation, Macrophages, and Severe COVID-19 Are Linked
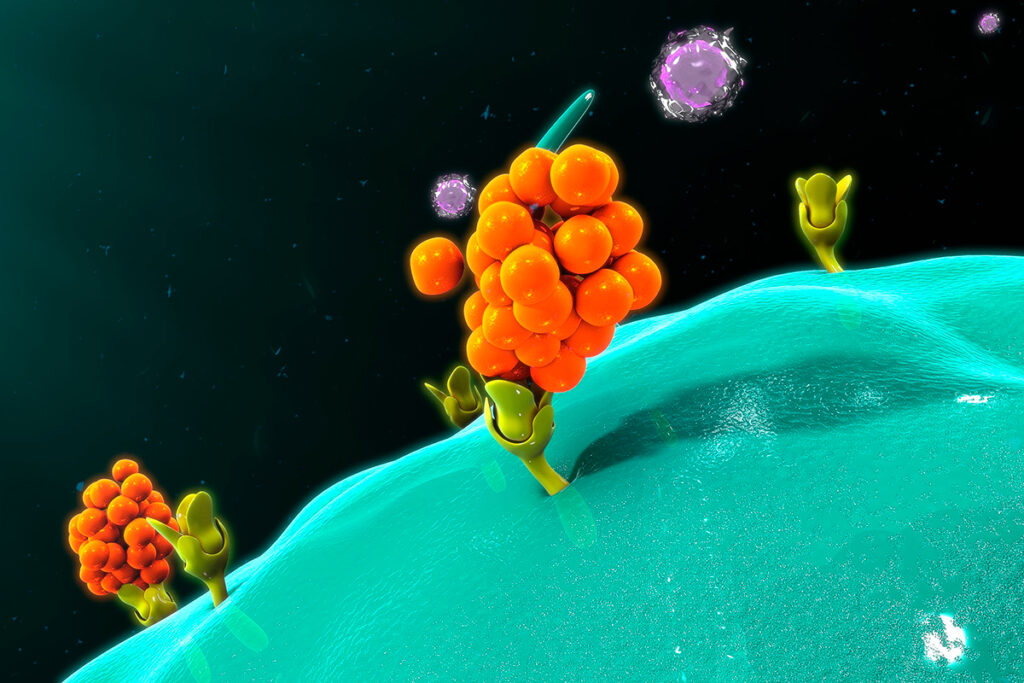
Monocytic macrophage cells play an essential role in the immunopathology of SARS-CoV-2. These cells launch a cytokine storm where interleukin IL-6 may play a unique role. This cytokine regulates the activation of monocytes, the differentiation of monocytes into macrophages, and the acquisition of inflammatory properties by macrophages.
Metabolic syndrome, obesity, type II diabetes, and cardiovascular disease are risk factors for severe COVID-19. All these conditions and diseases are closely associated with the activation of macrophages in an inflammatory manner. Inflammatory macrophages contribute to the development of indolent inflammation, which is recorded in patients with the above diseases. IL-6 is the driving force behind “metabolic inflammation”, and elevated levels of IL-6 are associated with the risk of severe COVID-19.
Interferon and ACE2
Angiotensin-converting enzyme 2 (ACE2) is the primary receptor for SARS-CoV-2 entry into the cell. Because studies have shown that IFNs can increase ACE2 expression, it has been suggested that IFN therapy may exacerbate COVID-19.
However, a recent study showed that interferons have an antiviral effect against SARS-CoV-2, and this antiviral effect balances the increase in ACE2 expression. Other studies have shown that under the influence of interferon, the expression of dACE2, an isoform of ACE2, to which SARS-CoV-2 cannot attach, increases.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary: