Most patients with COVID-19 coronavirus disease have mild symptoms, but some develop severe pneumonia. What factors cause a severe disease is not fully known. However, studies indicate an inadequate immune response and that coronaviruses may evade innate immunity. It is confirmed that patients with COVID-19 have a reduced type I interferon response (IFN), which is associated with impaired virus excretion. Ineffective elimination of SARS-CoV-2 can lead to uncontrolled tissue inflammation and death.
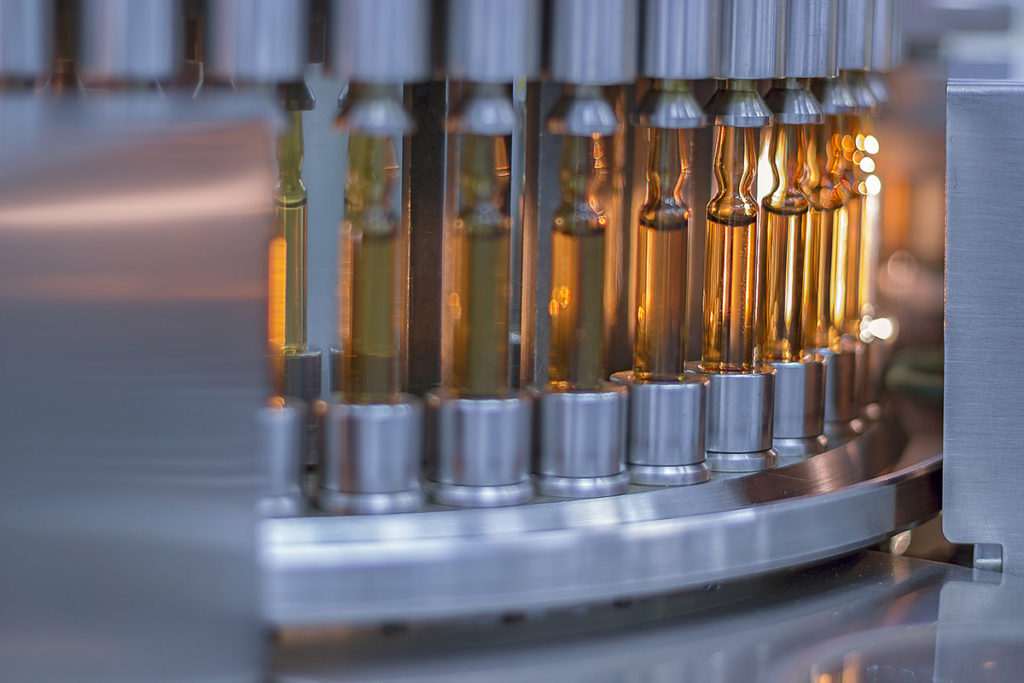
To date, there are no particular drugs for the treatment of COVID-19. The antimalarial drugs chloroquine and hydroxychloroquine have been suggested as prophylactic and therapeutic agents. These drugs inhibit the replication of the SARS-CoV-2 virus in vitro in primate cells. However, there is no evidence that these drugs can affect replicating the virus in the human body. Chloroquine and hydroxychloroquine also have immunomodulatory properties, which can affect the course of COVID-19 disease.
The immunomodulatory effects of hydroxychloroquine have been known for decades, and it is commonly used to prevent exacerbations of rheumatic diseases such as systemic lupus erythematosus and rheumatoid arthritis. This drug can inhibit the production of pro-inflammatory proteins-cytokines, such as IL-1β, IL-6, and TNF-α, by innate immune cells.
The use of chloroquine and hydroxychloroquine remains controversial, especially in the context of prevention. There is no clear evidence of the effectiveness or understanding of modus operandi. Dutch scientists investigated the immune response to COVID-19 and the immunomodulatory properties of hydroxychloroquine. They found out that interferon-stimulated genes are associated with severe coronavirus, and hydroxychloroquine can suppress trained immunity responses.
Trained immunity
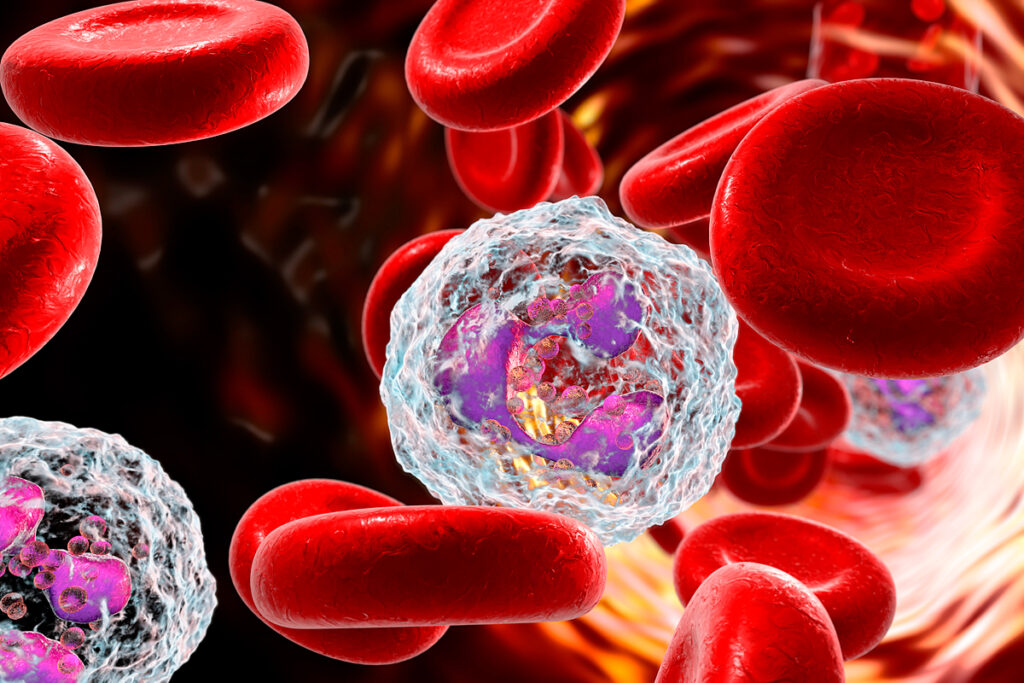
The immune system of vertebrates is traditionally divided into innate and adaptive. Cells in the innate immune system recognize pathogens and tissue damage through pattern recognition receptors (PRRs). When PRR is activated, rapid non-specific processes are activated: phagocytosis (uptake of solid particles by the cell), cell movement to the lesion site, destruction of pathogens or cells, and cytokine production. These innate immune mechanisms are usually very effective in eliminating invading pathogens. Also, dendritic cells (DCS) and specialized T-lymphocytes, and B-lymphocytes trigger adaptive immune responses that can be triggered simultaneously. These lymphocyte-dependent adaptive immune responses develop more slowly, but they are antigen-specific and lead to long-term immunological memory.
It was believed that immunological memory is an exceptional sign of an adaptive immune response for a long time. However, more and more studies confirm that innate immune cells can exhibit adaptive properties. Protection against reinfection – in fact, the function of immunological memory-is also present in plants and invertebrates, which do not have adaptive immunity. It demonstrates that the adaptation of the body’s defenses can occur based on innate immune mechanisms. Moreover, certain infections and vaccines can cause protection against a wide range of other pathogens through innate immune mechanisms. Conversely, the phenomenon of tolerance to an inflammatory stimulus is also an adaptation of cellular responses but leads to a lower inflammatory response to the second stimulation.
Damage caused by external and internal factors leads to long-term functional reprogramming of innate immune cells. Reprogramming of the cells leads to an altered response to the repeated stimulus after the cells return to an inactivated state. This property of the innate immune system to exhibit adaptive characteristics has been called trained immunity.
Changes in the cells of the innate immune system in COVID-19
Dutch scientists studied the immune response in patients with COVID-19 and compared it with a control group of healthy people. The study used peripheral blood mononuclear cells (PBMC) from 13 patients admitted to Radboud University Medical Center with SARS-CoV-2 infection.
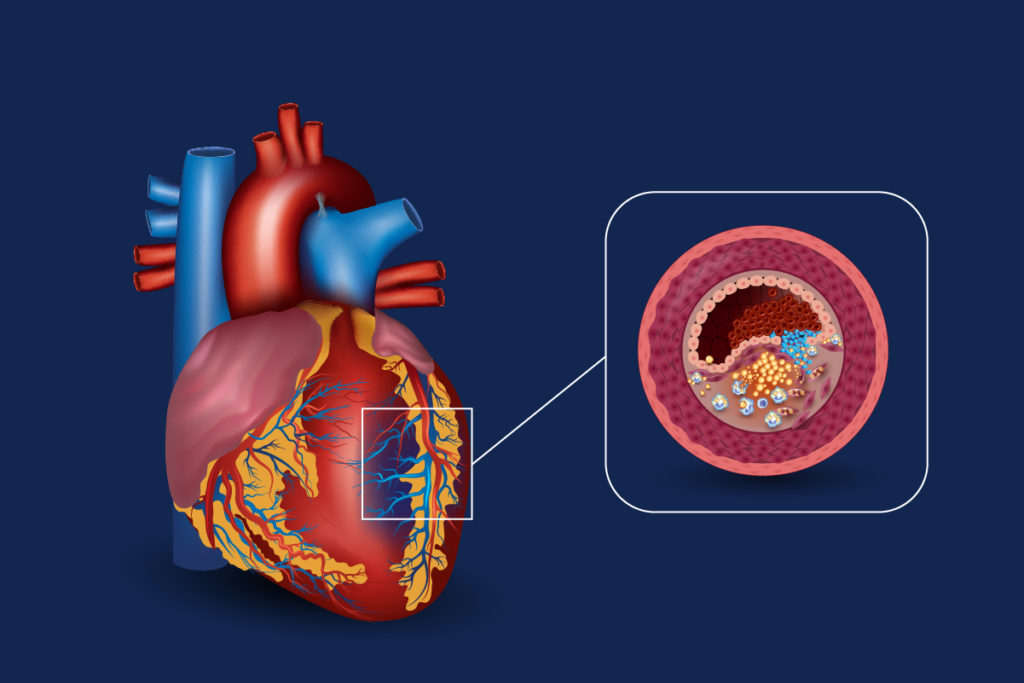
The study included patients over the age of 18 with a diagnosis of COVID-19. Blood was taken at admission and 5 days after admission from patients who remained hospitalized. Treatment with chloroquine was initiated upon admission and lasted for 5 days. The average age of patients is 68 years. 5 patients had a history of lung diseases, 3 had cardiovascular diseases, and 3 had malignant neoplasms. Most patients had a high fever (62%), cough (77%), and/or shortness of breath (54%). 7 out of 13 patients required additional oxygen therapy during treatment (<5 l / min). All the patients in the chest scans showed signs of pneumonitis. At the time of treatment, none of the patients was in critical condition.
The researchers analyzed subpopulations of immune cells. At the time of hospitalization, patients with COVID-19 had slightly fewer T-lymphocytes, but there were no differences in other lymphocytes’ subgroups. In patients with COVID-19, classical monocytes were markedly enlarged, while non-classical monocytes were virtually undetectable. Human leukocyte antigen DR (HLA-DR) was reduced in the monocytes of patients with COVID-19 – and in coronavirus, low HLA-DR expression is associated with monocyte hyperactivation excessive release of the pro-inflammatory protein interleukin-6 (IL-6). The subpopulations of lymphocytes and monocytes and HLA-DR manifestation did not change for 5 days in patients who remained hospitalized.
The researchers observed increased release of cytokines IL-1β, IL-6, and tumor necrosis factor-alpha (TNF-α) after PBMC stimulation for 24 hours with lipopolysaccharide, TLR2 agonist Pam3CSK4, and heat-killed Candida albicans (HKCA). This increased cytokine response did not change in patients who remained hospitalized during the 5-day follow-up period.
The researchers investigated whether changes in the innate immunity profile were related to altered responses in the adaptive immune system. For 7 days, the researchers stimulated PBMC with heat-killed Staphylococcus aureus (HKSA) and measured markers of activation of cells that enhance the adaptive immune response – T-helper cells: IFNy as a marker of activation of T-helper cells 1 (Th1) and IL-17 as a marker of activation of Th17. In the healthy control group, significant IFNy production and low IL-17 production were observed, indicating a dominant Th1 response. In contrast, in patients with COVID-19, IFNy production was reduced, and IL-17 production increased, indicating an increased Th17 response.
IFN-stimulated gene expression is associated with severe COVID-19
The researchers investigated what exactly differences in immune responses are related to the outcome of the disease.
Of the 13 patients with COVID-19, nine recovered without needing to be admitted to the Intensive care unit (ICU), three were required to be admitted to the ICU, and one died.
There were no clinical variables between patients who recovered and those who needed ICU or died at the time of hospitalization. No differences in white blood cell subpopulations were observed between the two groups, except for fewer B cells in patients who eventually required hospitalization in the ICU or died. HLA-DR monocytes’ expression was reduced, indicating that the monocytes’ inflammatory response was more pronounced in patients who required ICU or died.
The researchers analyzed the monocytes of patients with COVID-19 and found noticeable differences in the transcription of IFN-stimulated genes, which are crucial in the context of viral infections. Higher expression of IFN-stimulated genes was associated with possible ICU admission or death.
Six patients recovered quickly and were discharged within the first 5 days, while seven patients remained hospitalized. The researchers analyzed the PBMC of these seven patients 5 days after admission. No differences in the subpopulations of lymphocytes were observed. However, patients who required hospitalization in the ICU or died had more classic monocytes. The number of non-classical monocytes recovered in patients who recovered but remained virtually undetectable in patients who required hospitalization in the ICU or died. In the monocytes of patients who required hospitalization in the ICU or died, HLA-DR expression and the CX3CR1 receptor, which plays a vital role in monocytes’ survival, were reduced. In patients who required hospitalization in the ICU or who died, the IFN-stimulated genes’ transcription was increased 5 days after hospitalization.
Together, these findings suggest that the inflammatory response in SARS-CoV-2 infection is characterized by marked changes in the innate immune system. Monocytes show signs of increased activation and increased expression of IFN-stimulated genes, which are markers of disease severity, as they are associated with a poor outcome.
Scientists have identified an increased cytokine response of monocytes, which persists throughout the disease and resembles the inflammatory response in sepsis and influenza. The increased innate immune response indicates the reprogramming of innate immunity, contributing to the improvement of antiviral mechanisms and infection resolution.
Hydroxychloroquine prevents the formation of a trained immune system
In patients with COVID-19, the sensitivity of monocytes is increased. This functional adaptation of monocytes is also observed in such processes as priming (initial encounter with the pathogen) and the formation of trained immunity. These processes enhance the antiviral innate immune response.
Lysosomes are the parts of the cell that coordinate immune metabolism and the innate immune response. Chloroquine and hydroxychloroquine enter the lysosome and disrupt its functions. Scientists investigated whether chloroquine and hydroxychloroquine affect the trained immune system. The researchers observed that HKCA-stimulated PBMC produced significantly more cytokines when restimulated with either lipopolysaccharide (LPS) or Pam3CSK4. This effect disappeared when the cells were treated with chloroquine and hydroxychloroquine for 24 hours during HKCA stimulation. A similar result was observed when PBMC was exposed to a virus-like stimulus. This fact confirms that chloroquine and hydroxychloroquine prevent the formation of a trained immune system.
Chloroquine and hydroxychloroquine do not inhibit cytokine production in general. It is confirmed by the experience in which untrained monocytes were treated with chloroquine and hydroxychloroquine for 24 hours – cytokine production after LPS stimulation 5 days later did not change. Besides, when HKCA-trained PBMCs restimulated LPS with or without chloroquine and hydroxychloroquine treatment after 5 days of rest, cytokine production was also not suppressed.
IFNs play a central role in antiviral immune responses. In patients with COVID-19, the expression of IFN-stimulated genes is increased. The researchers investigated how inflammatory monocytes respond to restimulation of IFNa, IFNß, and IFNy. Increased production of pro-inflammatory cytokines IL-6 and TNF-α were observed. This effect was mitigated by treatment with chloroquine and hydroxychloroquine during the HKCA training stimulus.
Hydroxychloroquine prevents the increased expression of the genes encoding IL-1α and IL-1β, which play a central role in trained immunity. Treatment with hydroxychloroquine significantly suppresses genes, including IFN-stimulated genes associated with inflammatory responses.
Cholesterol synthesis is involved in the formation of a trained immune system. The creation of an introduced immune system is accompanied by profound changes in the lipid composition of monocytes. Hydroxychloroquine changes the lipid composition differently than when HKCA cells are stimulated without it.
Trained immunity is a functional adaptation of monocytes caused by their reprogramming and enhancing their immunological response. Hydroxychloroquine prevents the reprogramming of cells necessary to create a trained immune system. This study indicates that hydroxychloroquine reduces the trained innate immune response, including virus-like stimuli and IFN.
Conclusions
The use of chloroquine and hydroxychloroquine to treat COVID-19 remains a topic of intense discussion and research. Recently published studies found no positive effects of hydroxychloroquine in hospitalized COVID-19 patients. They were treated with hydroxychloroquine were more likely to require invasive mechanical ventilation or die.
Should chloroquine and hydroxychloroquine be used to prevent COVID-19?
The first randomized controlled trial on this topic, involving 821 patients, found that hydroxychloroquine as post-exposure prophylaxis did not prevent symptomatic SARS-CoV-2 infection. A follow-up study involving 132 health care workers in hospitals found that the use of this drug as pre-exposure prevention did not affect the incidence of SARS-CoV-2 disease.
This study shows that chloroquine and hydroxychloroquine prevent monocytes’ reprogramming and form a trained immune system. It is known that an introduced immune system enhances the innate immune response and thus contributes to the protection against infections. Previous research has shown that building a trained immune system, such as vaccinating against the Bacillus Calmette-Guerin (BCG), can help prevent bacterial and viral infections. The fact that chloroquine and hydroxychloroquine avoid trained immunity production shows that these drugs may not help treat viral infections such as SARS-CoV-2 and opposes their use as a prophylactic against COVID-19.
Sources
- Hydroxychloroquine Inhibits the Trained Innate Immune Response to Interferons
- Defining trained immunity and its role in health and disease