The development of a tumor is influenced by its microenvironment. The tumor microenvironment (TME) consists of the extracellular matrix, blood vessels, immune and other cells. The tumor and its TME constantly interact. This interaction influences disease progression and response to therapy.
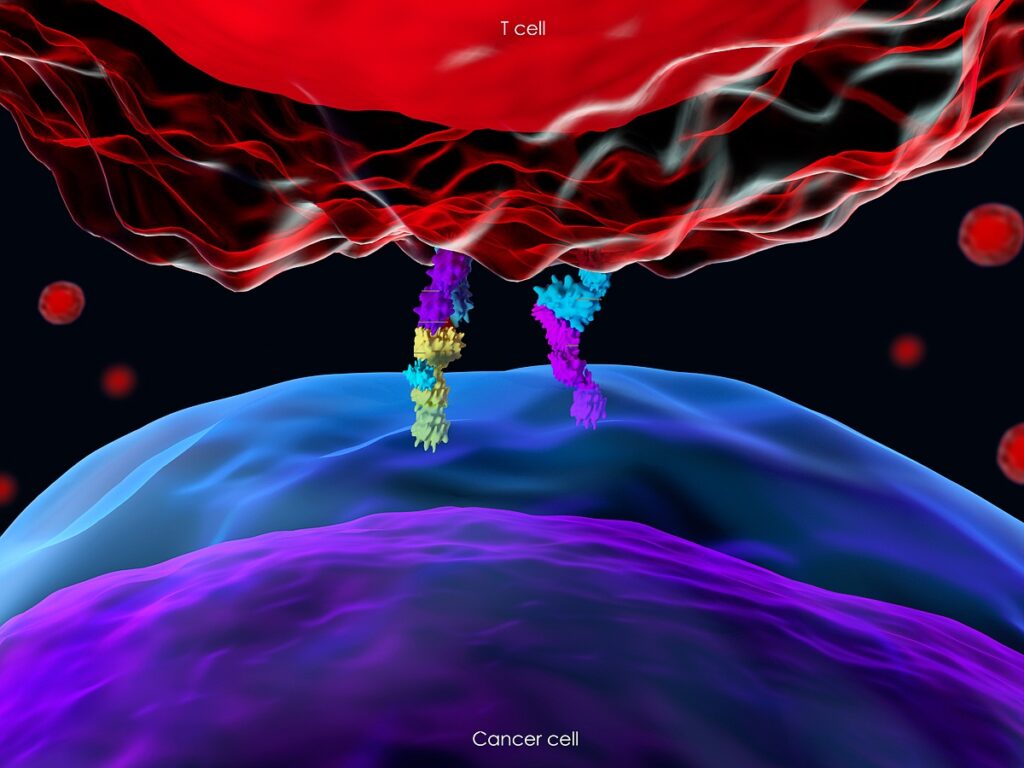
Immune cells are vital participants in the tumor microenvironment. They are the ones who know how to distinguish healthy cells from tumor cells to destroy only cells that are dangerous to the body. To do this, a receptor on the surface of a T-cell connects to a protein on the surface of a healthy cell, after which the T-cell receives a signal that it is a normal cell in front of it, and it should not be destroyed. This signal is called an immune checkpoint. Some tumor cells produce proteins that can also bind to the T-cell receptor. It prevents the immune system from destroying cancer.
One of the tumor treatments, immune checkpoint blockade (ICB), is based on drugs that prevent the T-cell receptor from binding to a partner protein. The T cell does not receive a signal that a healthy cell is in front of it and destroys the tumor. Unfortunately, ICB does not always help. The reason for this is that the tumor microenvironment suppresses the immune system.
The cells of innate immunity – mononuclear phagocytes (monocytes, macrophages, and dendritic cells) – play an essential role in TME. They have high plasticity and can both induce anti-tumor reactions and promote immunosuppression and tumor progression.
Monocytes can be divided into two main subsets: classical and non-classical. Both can play both positive and negative roles in cancer. If in TME they differentiate into macrophages, then the tumor will progress. Moreover, if in dendritic cells, an anti-tumor response will follow.
Intestinal Microbiota Affects Anti-Tumor Immunity and Response to Chemotherapy and Immunotherapy
The composition of the microbiota determines whether ICB cancer therapy is effective or not. A 2016 study found that gut microbiota affects the differentiation of mononuclear phagocytes.
Scientists at the US National Cancer Institute investigated how the microbiota regulates the functional state of mononuclear phagocytes in the tumor microenvironment.
Research results:
- For differentiation of mononuclear phagocytes into immunostimulatory monocytes and dendritic cells, TME requires signals derived from the microbiota. The absence of these signals promotes the differentiation of mononuclear phagocytes into tumor-stimulating macrophages.
- Intestinal bacteria produce the signaling molecule c-di-AMP, which activates the stimulator of the interferon genes STING and triggers the production of type I interferon (IFN-I) by intratumoral monocytes. IFN-I regulates the maturation of dendritic cells and the activation of NK cells (natural killer cells), which destroy the tumor.
- This mechanism can be triggered by exposing the microbiota through a high fiber diet (FD). Under the influence of FD, the intestinal bacterium Akkermansia muciniphila produces c-di-AMP. That triggers an IFN-I response and increases the number of dendritic cells.
- Scientists have confirmed the results of a study in people with melanoma who received ICB. Fecal microbiota transplantation from only ICB responsive patients is sufficient to trigger an IFN-I response and regulate TME innate immunity.
Conclusions
The microbiota influences the anti-cancer immune response.
Proteins that stimulate STING and are derived from the microbiota (for example, c-di-AMP) trigger the production of type I interferon by intratumoral monocytes. It promotes the anti-tumor response in the tumor microenvironment. IFN-I regulates the maturation of dendritic cells, recruitment, and activation of NK cells. If the microbiota is disturbed, this does not happen, and monocytes differentiate into proto-tumor macrophages.
Improving the microbiota with a high-fiber diet, monocolonization by Akkermansia muciniphila bacteria producing c-di-AMP, or systemic administration of c-di-AMP is sufficient to trigger the IFN-I response and enhance anti-tumor immunity.
Microbiota transplantation from patients who respond to ICB triggers an intratumoral IFN-I response, regulates the TME immune environment, and promotes ICB response.
Impact on innate immune cells through the microbiota will help eliminate the problem of the immunosuppressive tumor microenvironment.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Source
Microbiota triggers STING-type I IFN-dependent monocyte reprogramming of the tumor microenvironment