Helicobacter pylori bacterium has infected more than half of the world’s population. This bacterium is the leading cause of gastritis, ulcers, and stomach cancer. Scientists are still investigating the mechanisms that allow Helicobacter pylori to defend itself against the immune system and cause chronic infection.
One of the mechanisms was discovered in 2013 by an international team of scientists from the University of Copenhagen (Denmark) and Monash University (Australia). Scientists have found that the bacterium secretes the toxin VacA, which blocks the production of interferon-beta (IFN-β) stimulated by probiotics. So Helicobacter prevents the launch of adaptive immunity.
Research Background
Earlier studies conducted in 2010-2012 by the same group of scientists showed that the probiotic bacterium Lactobacillus acidophilus stimulates the production of IFN-β by immune cells. Moreover, L. acidophilus proved to be the most effective stimulant of all 46 probiotic strains studied.
Even earlier clinical and laboratory studies conducted in 2006-2007 in Switzerland, Italy, and Japan showed that using probiotics reduces Helicobacter pylori and the side effects of standard antibiotic treatment.
However, there is another 2011 study conducted by Portuguese scientists on patients with peptic ulcers and ulcerative scars. This study did not show the benefit of L. acidophilus in the treatment of Helicobacter pylori with two antibiotics at the same time.
Thus, in some cases, probiotics stimulate the production of interferon-beta and the launch of adaptive immunity against Helicobacter pylori, while in others, this does not happen for some reason. The aim of this study was formulated as follows:
- establish the reason for the lack of synthesis of IFN-β;
- determine the conditions under which the production of interferon-beta is still possible.
Study Design
For the experiments, the scientists used macrophages, the primary type of immune cells that destroy Helicobacter pylori. The second participant in the investigation is the probiotic bacterium L.acidophilus, which most effectively stimulates the production of interferon-beta by macrophages, followed by the launch of adaptive immunity.
Two types of Helicobacter bacteria have been used:
- wild type – for modeling the environment as close to natural as possible;
- genetically modified bacteria – for a detailed study of the interaction between probiotic bacteria and Helicobacter pylori.
Macrophages were sequentially stimulated at first only L. acidophilus, then only Helicobacter. Moreover, in conclusion – both types of bacteria are simultaneous. The scientists sought to identify differences in immune responses.
Results
Interferon-beta synthesis levels
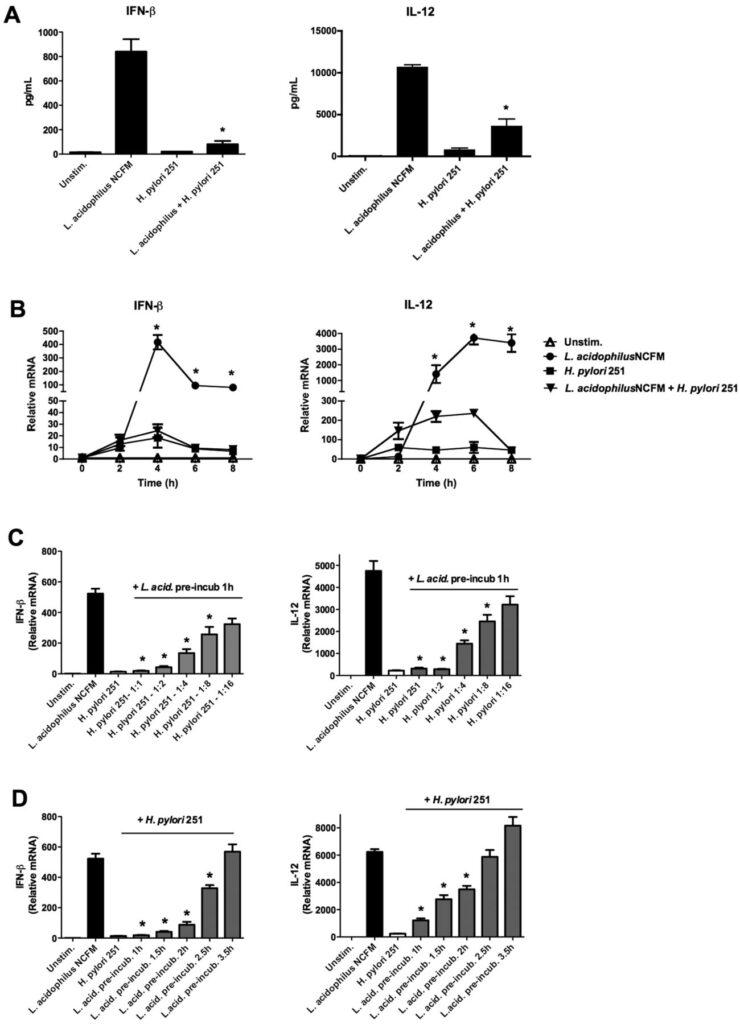
First, scientists were convinced that L. acidophilus could trigger interferon-beta production by macrophages. It turned out that 10 hours after adding the probiotic to macrophages, the level of IFN-β increased significantly to 840 pg/ml. Also, the level of another signal protein, IL-12, increases considerably up to 10,700 pg/ml, promoting immune cells’ maturation and triggering the production of immune defense proteins.
When macrophages were stimulated only by Helicobacter, the production levels of IFN-β and IL-12 were significantly lower – 20 pg/ml and 850 pg/ml, respectively.
In the next experiment, scientists observed the combined effect of different types of bacteria on macrophages. First, the scientists treated macrophages with a probiotic for one hour and then added wild-type Helicobacter pylori. As a result, after adding Helicobacter, the total interferon-beta production decreased by 90% and IL-12 by 66%.
The results are presented in the figure below (Graph. A).
Dynamics of Interferon-Beta Production
To determine the dynamics of interferon synthesis, scientists took measurements 2, 4, 6, and 8 hours after the start of the experiment. The maximum production of interferon-beta was achieved after 4 hours. Moreover, when macrophages were stimulated only by L. acidophilus, the synthesis volume increased 400 times compared with the control group. With stimulation, only Helicobacter pylori increased 15 times.
When Helicobacter was added to macrophages after stimulation with a probiotic, the production of IFN-β was blocked entirely, and the synthesis of IL-12 was reduced by 94%.
The results are presented in the figure below (Graph. B).
The Ratio of Helicobacter Pylori to Probiotic Restoring The Synthesis of Interferon
All previous experiments were carried out when the concentrations of Helicobacter pylori and L. acidophilus were the same (1:1). Therefore, scientists decided to establish at what ratio of probiotic to Helicobacter the synthesis of interferon-beta is restored. Experiments were carried out for cases where the concentration of the probiotic was 2, 4, 8, and 16 times higher than Helicobacter pylori.
Even at a concentration of 1:8, interferon-beta synthesis was 51% lower. Furthermore, only at a concentration of 1:16, the effect of Helicobacter becomes insignificant.
The results are presented in the figure below (Graph. C).
Scientists have suggested that the reason is not in the negative impact of a single bacterium but in the substances that Helicobacter produces to suppress the immune system.
Period of Macrophages Stimulation with a Probiotic to Reduce The Negative Impact of Helicobacter pylori
After 1.5 hours of stimulation with a probiotic and after the addition of Helicobacter following the stimulation, the production of IFN-β decreased by 92%. After 2 hours – it fell by 83%, and after 2.5 hours – by 63%. The negative effect on the synthesis of IFN-β completely stopped after 3.5 hours.
The results obtained are presented in the figure below (plots D).
Drawing:
Image source: https://journals.asm.org/doi/full/10.1128/mBio.00609-12
Genetic analysis of macrophages stimulated by Helicobacter pylori or L.acidophilus
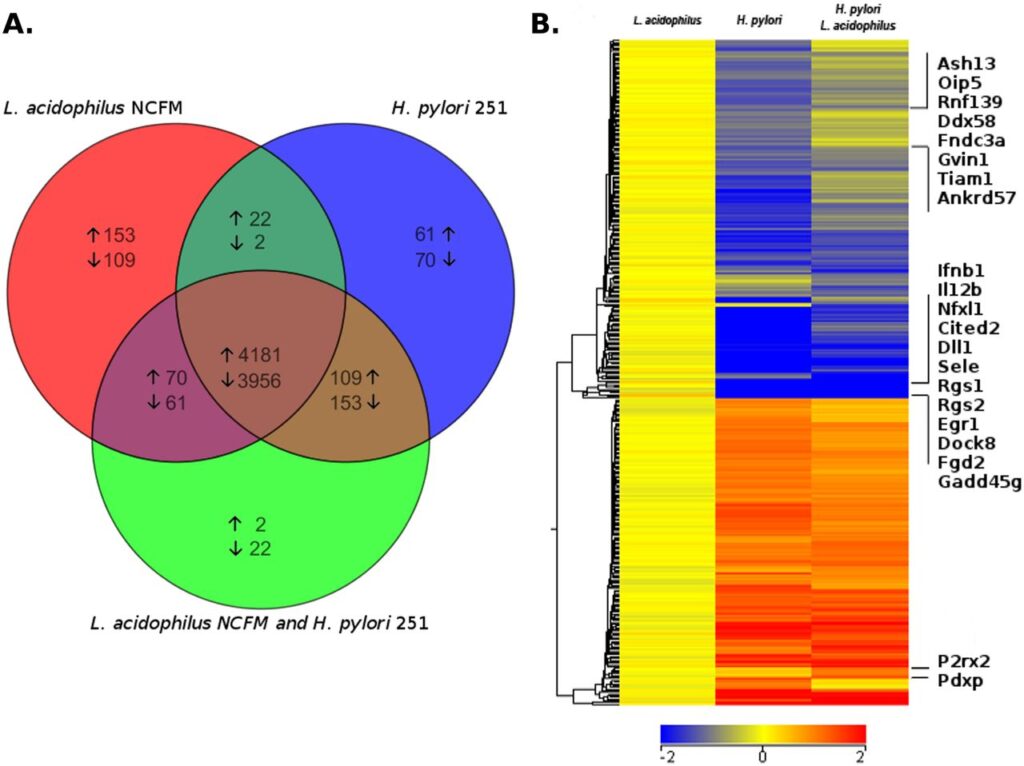
To assess the scale of influence of Helicobacter, scientists calculated the number of macrophage genes activated or suppressed in the case of:
- stimulation only acidophilus;
- stimulation only Helicobacter pylori;
- joint stimulation of Helicobacter pylori and acidophilus at a concentration of 1:1.
In all cases, the activity of 4,181 genes increased, and 3,956 genes decreased. Stimulation of L. acidophilus increased the activity of genes responsible for adaptive immunity. In particular, innate immunity genes that promote adaptive immunity development were stimulated, including genes associated with interferon-beta synthesis.
When stimulated by the bacterium Helicobacter, genes responsible only for innate immunity were activated, and adaptive immunity genes were suppressed:
Image source: https://journals.asm.org/doi/full/10.1128/mBio.00609-12
A Toxin that Helps Helicobacter Inhibit The Synthesis of IFN-β is Revealed
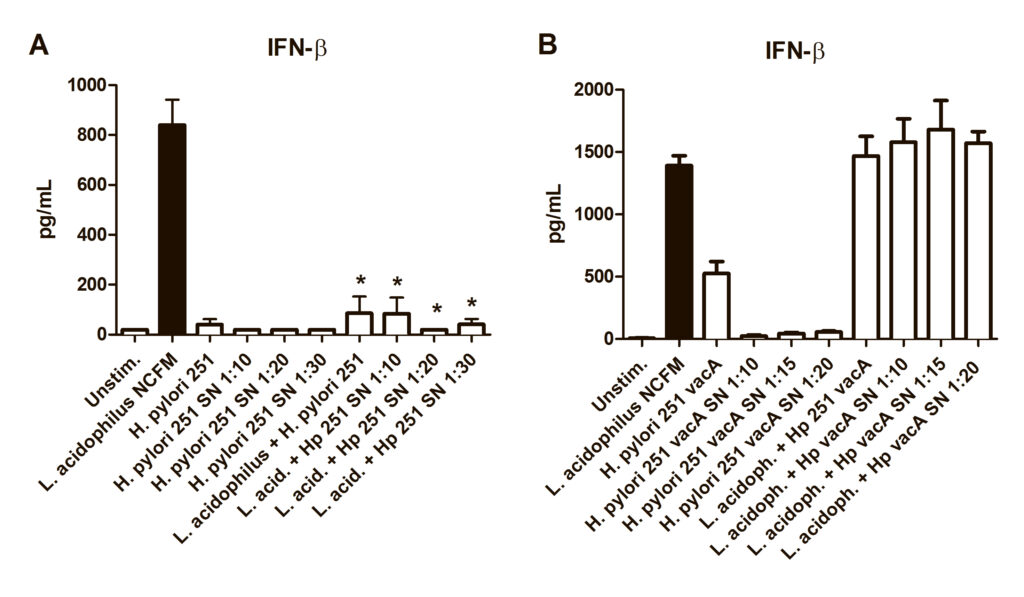
In 2000, scientists from the University of Birmingham (Great Britain) investigated the effect of the VacA toxin produced by Helicobacter pylori on epithelial cells. VacA toxin contributed to the formation of acidic vacuoles in cells and disruption of the structure of the cell membrane, which worsened the protective properties of the mucus lining the stomach.
In the present study, the scientists hypothesized that the same VacA toxin could suppress the production of IFN-β in macrophages. To test the hypothesis, scientists used a genetically modified strain of Helicobacter, which cannot produce the desired toxin. The genetically modified strain does not affect the synthesis of interferon-beta, unlike wild-type Helicobacter:
Image source: https://journals.asm.org/doi/full/10.1128/mBio.00609-12
Conclusions
Probiotics reduce the number of Helicobacter pylori. The effect is based on stimulating protein production that triggers adaptive immunity, particularly interferon-beta.
However, Helicobacter can suppress the positive effect of probiotics and block the synthesis of IFN-β. The negative impact is leveled when the number of probiotic bacteria is 16 times higher than that of Helicobacter. Interferon production is also not blocked if immune cells are pre-treated with a probiotic for 3.5 hours.
The mechanism by which Helicobacter disrupts the synthesis of IFN-β is based on the production of the toxin VacA. This toxin forms acidic vacuoles in immune cells and disrupts the structure of cell membranes. A genetically modified strain of Helicobacter, which cannot synthesize the VacA toxin, cannot block interferon-beta production.
References
- Helicobacter pylori VacA Suppresses Lactobacillus acidophilus-Induced Interferon Beta Signaling in Macrophages via Alterations in the Endocytic Pathway
- MyD88 Drives the IFN-β Response to Lactobacillus acidophilus in Dendritic Cells through a Mechanism Involving IRF1, IRF3, and IRF7
- Helicobacter pylori and Probiotics
- Lactobacillus reuteri therapy to reduce side-effects during anti-Helicobacter pylori treatment in children: a randomized placebo controlled trial
- Effect of Bifidobacterium bifidum Fermented Milk on Helicobacter pylori and Serum Pepsinogen Levels in Humans
- Lactobacilli and bifidobacteria induce differential interferon-β profiles in dendritic cells