Lactobacilli and bifidobacteria are commonly called probiotics because they promote health. They help maintain the intestinal epithelium’s integrity and suppress pathogenic microorganisms’ growth. Probiotics positively affect both the local immunity of the digestive tract and the body’s overall immunity. Probiotics treat inflammatory bowel disease, atopic dermatitis in children, and other allergic manifestations and prevent viral infections.
Despite the successful clinical use of lactobacilli and bifidobacteria, how a specific type and strain affects the immune system is unclear. Scientists from the University of Copenhagen (Denmark) studied the effects of 43 strains of probiotics on vital immune cells of the intestine – dendritic cells. These cells extend their dendrites through the dense intestinal epithelium and interact directly with the microbiota, sampling genes. Depending on the type of samples received, dendritic cells synthesize immune signaling molecules, particularly interferon-beta (IFN-β, IFN-β).
Study Design
The scientists used bacteria derived from the microbiota of the gastrointestinal tract. All selected 27 strains of lactobacilli and 16 strains of bifidobacteria are used in dairy production:
| Lactobacilli (Lactobacillus) | |
| Type | Number of studied strains |
| L. casei | 6 |
| L. acidophilus | 2 |
| L. gasseri | 1 |
| L. plantarum | 4 |
| L. paracasei | 5 |
| L. paraplantarum | 1 |
| L. reuteri | 3 |
| L. rhamnosus | 4 |
| L. ruminus | 1 |
| Bifidobacteria (Bifidobacterium) | |
| Type | Number of studied strains |
| B. bifidum | 5 |
| B. breve | 3 |
| B. longum | 6 |
| B. infantis | 1 |
| B. animalis | 1 |
Scientists isolated dendritic cells from mouse bone marrow, added one or several strains of probiotics to them, and studied the dynamics of the synthesis of signaling immune proteins. In preliminary experiments, with an increase in the concentration of probiotics, the production of signaling proteins first increased, then reached a maximum, and then decreased.
Research Results
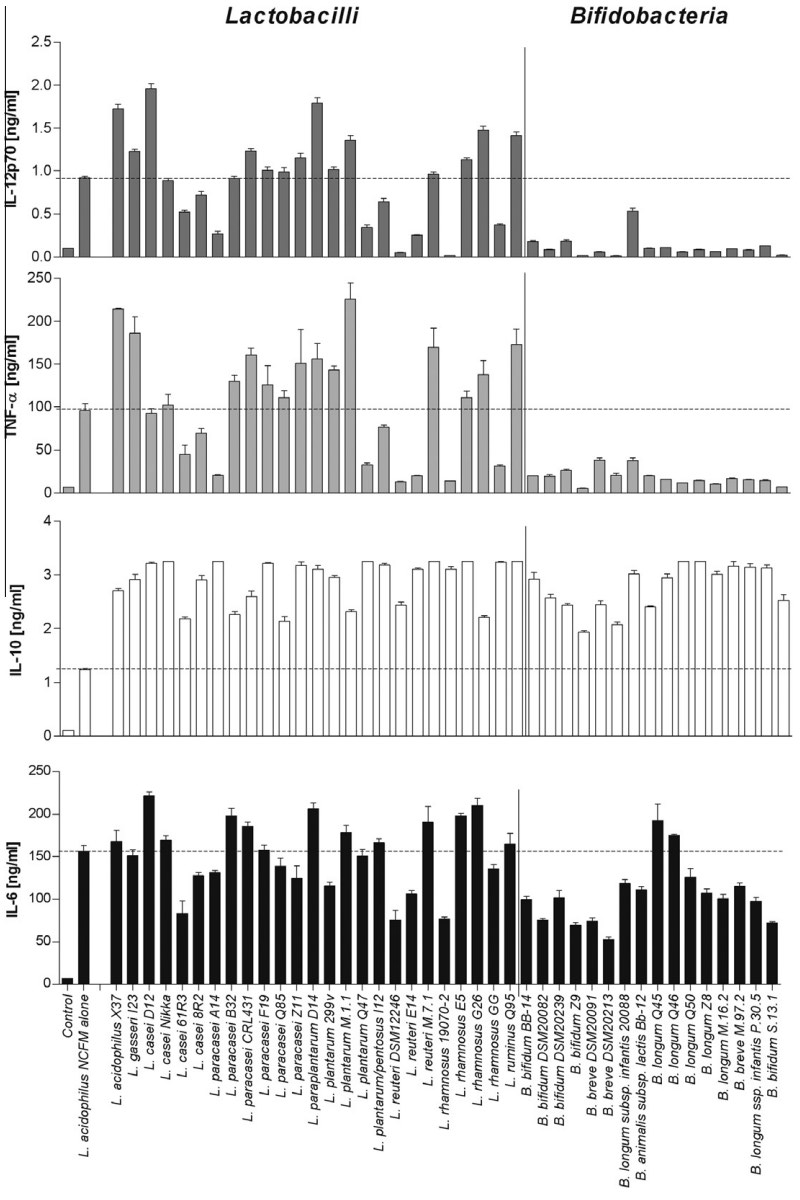
Scientists have found that different strains differ in the amount of synthesized signaling immune proteins and their composition.
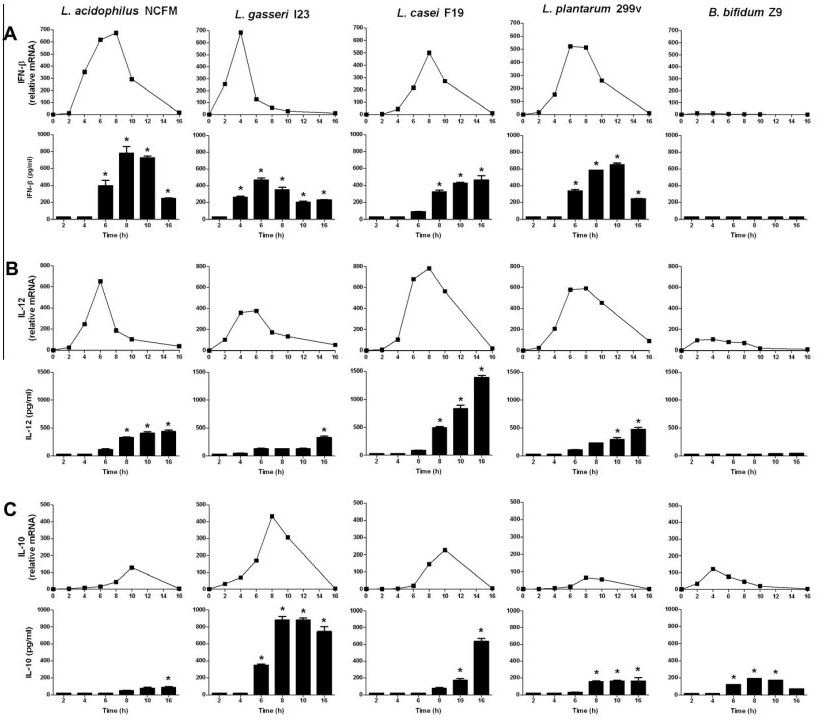
About half of the representatives of the Lactobacillus genus – Lactobacillus acidophilus, L. casei, L. plantarum, and L. gasseri – promoted the production of a large number of antiviral defense proteins. Primarily interferon-beta stimulates the innate and adaptive immune system to prevent and fight viral infections. These bacteria also trigger the production of proteins in dendritic cells that promote inflammatory reactions and attract other immune cells to infected areas to fight pathogens. Strains of L. acidophilus stimulated the highest synthesis of IFN-beta. L. casei and L. plantarum produced a slightly lesser amount. On average, the maximum interferon-beta production was reached in 6-8 hours, which began to decrease. L. gasseri bacteria stimulated the production of a significantly smaller amount of IFN-beta, but this happened faster – the maximum amount was reached in 4 hours, and within 6 hours, it quickly decreased.
All of these bacteria stimulated the production of signaling proteins that promote inflammation:
- IL-12 – encourages the maturation of immune cells and triggers the production of other pro-inflammatory proteins;
- TNF-α – initiates inflammatory processes in various types of cells. It has both local and systemic effects;
- IL-6 – initiates the acute phase of inflammation, moving from damaged tissues to the liver and stimulating the production of other pro-inflammatory proteins.
The other investigated lactobacillus – L. reuteri, L. rhamnosus, L. paracasei, and L. paraplantarum – could not stimulate interferon-beta production but suppressed it. These bacteria synthesize proteins that suppress inflammation, promote wound healing, and regulate autoimmunity.
L. reuteri, L. rhamnosus, L. paracasei, and L. paraplantarum promoted the production of the signaling protein IL-10, which suppresses inflammation. IL-10 is a critical anti-inflammatory molecule that protects against excessive inflammatory reactions to pathogens. It is involved in wound healing and the regulation of autoimmunity.
All investigated strains of Bifidobacterium demonstrated a similar anti-inflammatory response.
The graph below shows the dynamics of IFN-beta and other signaling immune proteins produced under the influence of certain types of bacteria:
Image source: https://www.sciencedirect.com/science/article/abs/pii/S1043466611002572
The absolute values of the produced pro-inflammatory and anti-inflammatory signaling proteins are shown in the graph below:
Image source: https://www.sciencedirect.com/science/article/abs/pii/S1043466611002572
After experiments with the stimulation of dendritic cells using one strain of probiotics, scientists started combining strains. Strains that stimulate interferon-beta production were mixed with strains that suppress it. As a result, it was found that bifidobacteria and lactobacilli, which have similar functions, suppress the production of IFN-β even when stimulated by the most potent IFN-increasing strain, L. acidophilus.
Based on a series of experiments, scientists drew the following conclusions:
- Lactobacilli can be divided into two groups with opposite properties: those that stimulate inflammation and those that suppress it;
- It is crucial to choose the right strain for probiotic purposes;
- Their phylogenetic properties do not support the modern classification of lactobacilli.
Conclusions
Lactobacilli and bifidobacteria strengthen health, boost immunity, and prevent and treat diseases. However, these microorganisms affect the interferon system and inflammatory reactions differently. Bifidobacteria and some lactobacilli suppress the production of interferon-beta, promoting wound healing. Other lactobacilli, on the contrary, promote the synthesis of IFN-β and maintain antiviral activity, promoting inflammation. These characteristics should be taken into account when using probiotics.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
References
- Lactobacilli and bifidobacteria induce differential interferon-b profiles in dendritic cells
- Interleukin-12 and the regulation of innate resistance and adaptive immunityInterleukin-12 and the regulation of innate resistance and adaptive immunity
- Transmembrane TNF-α: structure, function and interaction with anti-TNF agents
- Biology and therapeutic potential of interleukin-10
- IL-6 in Inflammation, Immunity, and Disease