Patients with COVID-19 often suffer from elevated blood glucose levels – hyperglycemia. The disease disrupts the endocrine cells that produce insulin. The body regulates glucose levels worse, and patients develop insulin resistance, decreasing the sensitivity of tissues to insulin. In non-diabetic patients hospitalized with normal glycated hemoglobin, various disorders of glucose metabolism and dysfunction of insulin-producing cells were observed as a result of coronavirus infection. Several studies from Italy have shown that patients with COVID-19 and hyperglycemia are at high risk of death.
The SARS-CoV-2 coronavirus causes systemic inflammatory processes in the body, which increase insulin resistance and cause hyperstimulation of cells that synthesize insulin. It leads to a deterioration in the functioning of cells and their death. If the coronavirus enters the systemic circulation, it primarily infects the cells producing insulin when the pancreas is infected. As a result, patients with no prior medical history or diabetes have glycemic abnormalities.
A group of scientists from universities and medical centers in the United States and Italy conducted a study to demonstrate how hyperglycemia develops during the acute phase of coronavirus infection. The scientists also estimated how long glycemic abnormalities persist in patients who recovered from COVID-19.
Specialists observed 551 patients admitted with COVID-19 to the Fatebenefratelli-Sacco Hospital, Milan (Italy) from 02/01/2020 to 05/15/2020. The diagnosis of coronavirus infection was confirmed by PCR analysis of respiratory samples.
Research Results
Many cases of new-onset hyperglycemia in COVID-19
As a result of coronavirus infection, 46% of study participants (252/551) were diagnosed with hyperglycemia for the first time. Moreover, persistent hyperglycemia continued to be observed for 6 months in 35% of these people. Diabetes developed in 2%. In the remaining 65% of cases, remission occurred, and glucose levels returned to normal.
Abnormal glycated hemoglobin levels were found in 27% of hospital admission (151/551). These people had a history of diabetes, or the diagnosis of diabetes was made during hospitalization.
Glucose levels remained normal in 27% of those admitted to the hospital (147/551).
The demographic and clinical parameters of the study participants are presented in the table:
| Total participants | Diabetes | Hyperglycemia | Normal glucose | |
| Number | 551 | 123 | 253 | 147 |
| Sex M/F (%) | 344 / 207 (62 / 38) | 103 / 48 (67 / 33) | 159 / 94 (65 / 35) | 82 / 65 (51 / 49) |
| Age | 67 ± 1,1 | 61 ± 0,9 | 61 ± 0,7 | 55 ± 1,5 |
| Body mass index (kg / m2) | 27 ± 0,5 | 29 ± 1,4 | 27 ± 0,7 | 27 ± 1,1 |
| With hypertension | 164 | 66 | 68 | 30 |
| Days to clinical improvement | 14,9 ± 0,5 | 20,2 ± 1,3 | 13,6 ± 0,6 | 12,8 ± 0,8 |
| Deaths (%) | 85 (15) | 42 (28) | 29 (11) | 14 (9) |
| Days to death | 11,4 ± 1,4 | 10,5 ± 2,1 | 11,7 ± 1,8 | 12,0 ± 1,9 |
| Marker of systemic inflammation interleukin-6, pg / ml | 79,1 ± 7,4 | 108,2 ± 18,7 | 74,6 ± 8,0 | 45,5 ± 9,5 |
Scientists note that frequent consequences of newly-onset hyperglycemia in patients with COVID-19 are prolonged hospitalization, deterioration of clinical parameters, a higher need for oxygen support, mechanical ventilation, and hyperglycemia for many months.
Continuous Glucose Monitoring Reveals Glycemic Abnormalities In COVID-19 And After Illness
To obtain detailed information about the glycemic status of patients, the researchers performed comprehensive glycemic profiling twice. The first time was during the acute phase of COVID-19. The second time – 62 ± 6.5 days after the onset of the disease. Each time, the analysis was carried out for 7 days. The retrospective analysis was conducted in an environment where neither the patients nor the medical staff knew the results. Continuous glucose monitoring was performed using the professional Medtronic Envision Pro CGM system, Medtronic Minimed, approved for use in the European Union.
The analysis was carried out in groups of patients:
- with acute COVID-19 (10 people);
- survivors of COVID-19 (10 people);
- a control group of people with type 2 diabetes, but without COVID-19 (10 people);
- a control group of healthy people without diabetes and COVID-19 (15 people).
The graphs show data for:
- a glucose level of 140 mg/dl, which the WHO establishes as an indicator of early diabetes;
- blood glucose levels 60 minutes and 120 minutes after meals.
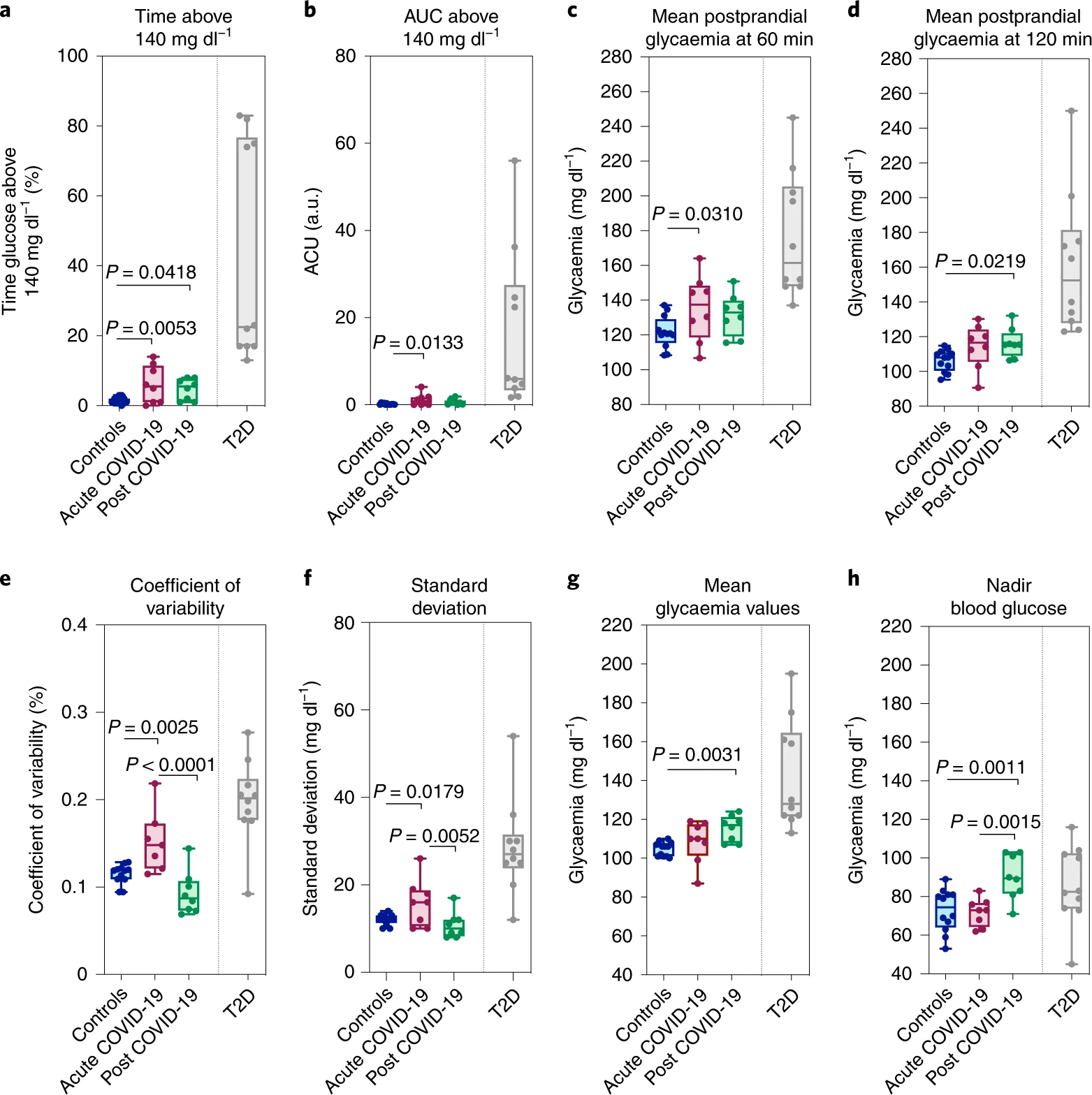
Continuous monitoring results show abnormal glucose levels in COVID-19 patients that persist even after the illness. However, this level is less than that of people with type 2 diabetes (T2D).
Scientists note that COVID-19 causes a long-term disruption of the glycemic profile at a glycemic level above 140 mg/dL (graph a). Compared to the healthy control group, patients with coronavirus infection significantly overestimated mean glycemia 60 minutes after eating (graphs c, d).
The surprise of scientists was caused by the persistence of hyperglycemia in some patients after recovering from COVID-19. Patients had glycemic levels above 140 mg / dL longer than healthy subjects. COVID-19 survivors also had higher blood glucose levels 120 minutes after a meal (graph d) and higher mean blood glucose levels (graph g).
Experts emphasize that one of the study’s main findings is that continuous monitoring of glucose levels can detect changes in glucose homeostasis that are not seen in a fasting blood test.
Insulin Resistance and Hyperstimulation of Insulin-producing Cells in COVID-19
Experts assessed the degree of insulin resistance and abnormalities in the cells that produce insulin. The researchers analyzed fasting and post-arginine serum hormones in a subset of patients who underwent continuous glucose monitoring.
The hormonal profile under fasting conditions (fasting) was analyzed using the following parameters:
- insulin levels;
- proinsulin level;
- the level of C-peptide – the result of the breakdown of proinsulin;
- assessment of dysfunction of β-cells of the pancreas for insulin production based on the Homeostatic Model Assessment β-cell (HOMA-B);
- the index of insulin resistance based on the homeostasis model -Homeostatic Model Assessment for Insulin Resistance (HOMA-IR).
As a result, patients with COVID-19 had significantly increased all indicators than healthy people from the control group. The exception was the insulin-proinsulin ratio, which differed without statistical significance.
The picture was similar when stimulated with arginine. Patients with COVID-19 had significantly higher peak rates than healthy people. The exception is the level of C-peptide, which in the group of people who had been ill was similar to the level in the healthy control group.
The final result is clearly shown in the graph:
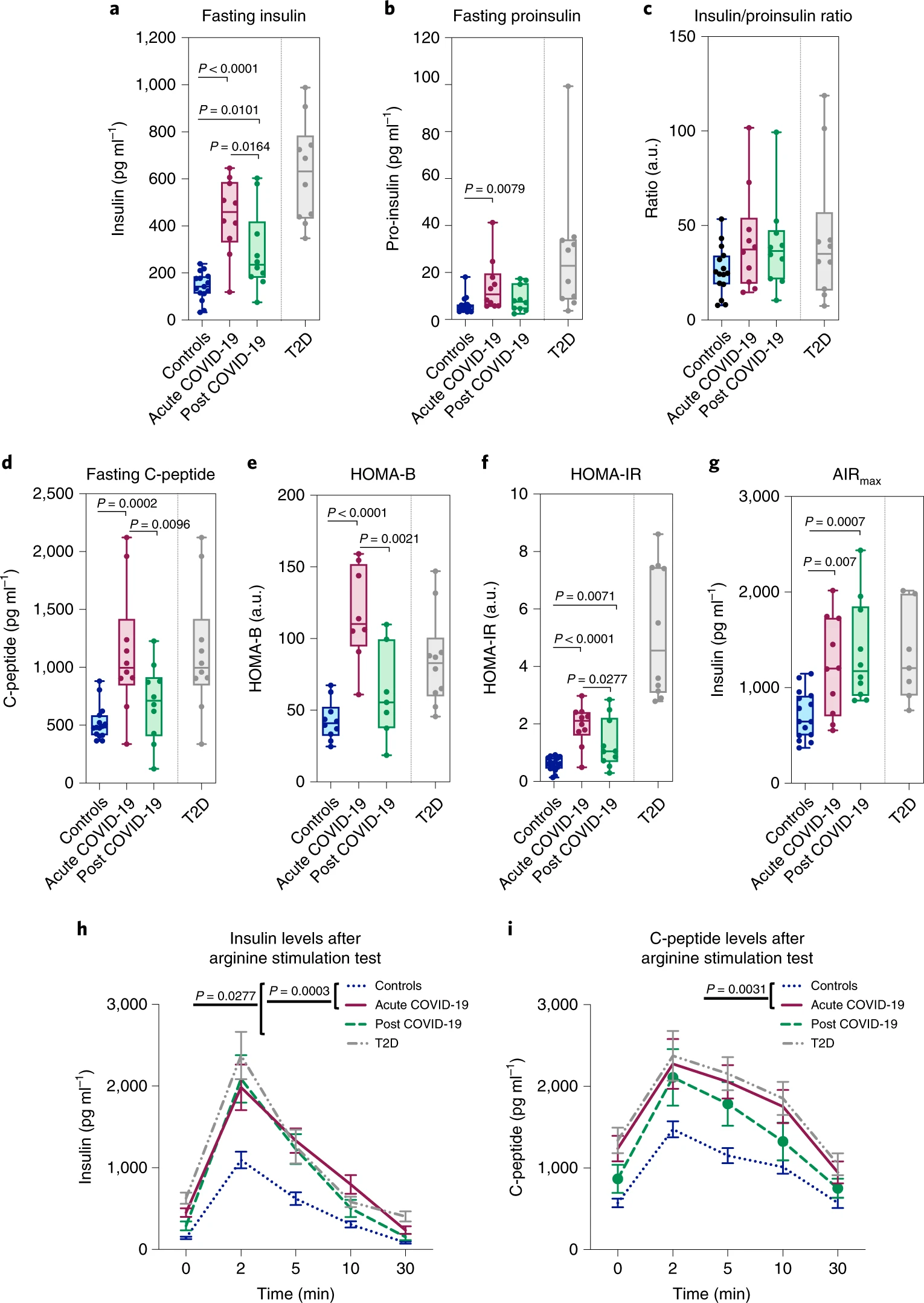
The data obtained show that in patients with acute COVID-19 and recovered patients, the hormonal profile remains overestimated both under fasting conditions and under stimulation with arginine. In this group of patients, persistent insulin resistance is observed, and their hormonal profile is similar to that of people with type 2 diabetes.
Scientists note that signs of β-cell hyperstimulation in patients with coronavirus infection and people who have had the disease can ultimately deplete the population of these cells and lead to their death.
Conclusions
The SARS-CoV-2 coronavirus disrupts glucose regulation in those who have fallen ill and recovered from COVID-19. In terms of their hormonal profile, these people are similar to those with type 2 diabetes. The coronavirus causes insulin resistance, disrupts insulin-producing cells, and depletes them in the body.
Glycemic changes in patients are recorded in the acute phase of COVID-19 and months after remission. Scientists believe that people who have had an illness need long-term monitoring of blood glucose levels.
Source
Acute and long-term disruption of glycometabolic control after SARS-CoV-2 infection



