Content
- Shape Anomalies
- Nail attachment anomalies
- Surface anomalies
- Color anomalies
- Nail abnormalities in organs
- Reference
Nail anomalies may be associated with systemic diseases. Therefore, the condition of the nails can help diagnose serious diseases before their first clinical manifestations occur. Fingernails usually provide more accurate information than toenails because toenails often change due to injury.
Shape Anomalies
Koilonychia – Concave Spoon-Shaped Nail Deformity
The early stage of koilonychia is the flattening of the nail. Koilonychia can occur either without specific causes or due to injuries or be the result of conditions such as:
- iron deficiency anemia is the most common cause;
- malnutrition;
- hemochromatosis – excessive accumulation of iron;
- cardiac ischemia;
- diseases of the thyroid gland;
- malignant neoplasms of the upper gastrointestinal tract.
Koilonychia is common in young children but often disappears in the first years of life. Also, koilonychia can occur in older adults due to a deterioration in the blood supply to the fingers, leading to thinning of the nails.
Figure 1. Fingernails in koilonychia and trachyonychia (dull, rough nails)
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Drum Sticks Symptom
The symptom of drumsticks is characterized by a thickening of the terminal phalanges of the fingers and an increased curvature of the nail plate in the longitudinal and transverse directions. The symptom may occur with such diseases as:
- congenital heart defects;
- infective endocarditis;
- lung cancer, pleural cancer;
- bronchiectasis;
- lung abscess;
- cystic fibrosis;
- inflammatory bowel disease;
- cirrhosis of the liver.
Drumsticks can also be an early sign of AIDS in HIV-positive children.
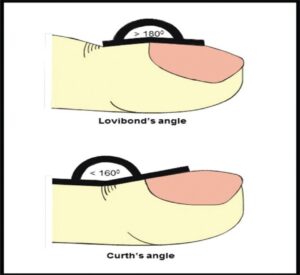
The deformation of the nails with a symptom of drumsticks is evaluated according to three signs:
- The Lovibond angle at the junction of the nail plate and the nail fold increase to more than 180° and usually is less than 160°.
- The Kurt angle between the middle and nail phalanges decreases to less than 160°, usually approximately 180°.
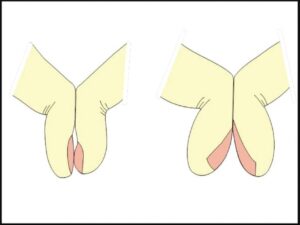
- Sign of Shamroth – the absence of a diamond-shaped space between the nail phalanges when the nails of the index fingers of the left and right hands are connected.
Figure 2. Lovibond angle and Kurt angle for clubbing symptom
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Figure 3. Shamroth’s sign: normal diamond-shaped lumen and its absence with a symptom of drumsticks
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Ingrown Nails
Nails grow into the nail folds when the transverse curvature of the nail increases. Large transverse curvature of the nail can be both a hereditary property and a consequence of diseases. Some of the causes of ingrown nails include:
- benign tumors under the nail bed and benign tumors of the nail matrix;
- end-stage renal disease associated with diabetes.
Dolichonychia
With dolichonychia, the length of the nail is much greater than its width. Causes include Marfan syndrome and hypothalamic-pituitary insufficiency.
Brachyonychia
With brachyonychia, the width of the nail plate is more significant than its length. Brachyonychia occurs in hyperparathyroidism and psoriatic arthropathy as an early sign of bone resorption.
Beak Nails
Symmetrical curvature of the free edge of the nails, similar to the parrot’s beak, is often associated with severe acrosclerosis with resorption of the nail phalanx due to scleroderma. As a result, the nail plate bends around the shortened fingertip.
Macronychia and Micronychia
Too big or too small nails compared to neighboring ones. Macronychia can be caused by local gigantism, and micronychia by tumors of the myelin sheath of neurons.
Nail Attachment Anomalies
Onycholysis – detachment from the nail bed
Areas of flaking appear white or yellow due to the space under the nail. Often, onycholysis is associated with trauma, psoriasis, fungus, and nail cosmetics reactions. However, sometimes onycholysis occurs with systemic diseases such as:
- anemia;
- brochiectasis;
- lungs’ cancer;
- cutaneous T-cell leukemia;
- diabetes;
- diseases of the thyroid gland;
- porphyria;
- systemic lupus erythematosus;
- psoriatic arthritis;
- T-cell lymphoma of the skin;
- taking psoralens and tetracyclines;
- vitamin C deficiency.
With thyrotoxicosis, the line of the detachment of the nail is straightened, then plunges into the nail bed in the form of a jagged protrusion.
Figure 4. Onycholysis in a patient with thyroid disease
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Pterygium – An Overgrowth of Nail Fold with its Adherence to the Nail
Pterygium results from scarring of the nail fold that extends into the matrix. Pterygium often occurs when:
- lichen planus;
- burns;
- pemphigus;
- congenital violation of keratinization of the upper layer of the skin;
- graft-versus-host reactions;
- radiation dermatitis;
- systemic lupus erythematosus.
In addition, pterygium is seen in leprosy, neurofibromatosis, benign tumors under the nail bed, and systemic sclerosis.
Figure 5. Pterygium on the second and third nails in lichen planus
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Surface Anomalies
Onychorrhexis – the Longitudinal Splitting of the Nail
Onychorrhexis looks like longitudinal depressed grooves or protruding ridges on the nail plate. A crack on one nail is most often associated with trauma. However, there is a connection between the longitudinal splitting of the nail and systemic diseases such as:
- amyloidosis;
- patella nail syndrome, accompanied by kidney pathology;
- collagen vascular pathology;
- graft-versus-host reaction;
- rheumatoid arthritis.
Combs down the center of the nail can cause iron, folic acid, or protein deficiencies.
Figure 6. Longitudinal nail splitting associated with severe anemia
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Beau’s Lines
Beau’s lines are transverse furrows extending from one edge of the nail to the other, which is the most common nail change in various systemic diseases. Among the reasons for the appearance of Beau’s lines are the cessation of nail growth due to injury, frostbite, psychological stress, malnutrition, fever, and heart attack.
The presence of Beau lines on all nails indicates systemic diseases such as:
- mumps (mumps);
- pneumonia;
- coronary thrombosis;
- Kawasaki disease;
- syphilis;
- hypoparathyroidism.
If the growth of the nail stops entirely within two weeks, the Beau line reaches its maximum depth, leading to nail detachment from the cuticle – onychomadesis.
Figure 7. Multiple lines of Beau on the middle finger and onychomadesis on the index finger
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Dull, Rough Nails (Trachyonychia) and Nail Ulceration
Pits on the nails occur due to a violation of the keratinization of the matrix. It is challenging to assume any specific disease from the pits on the nails because many different factors affect the matrix. However, the roughness of the nails and pits on the nails are found in diseases such as:
- psoriasis;
- psoriatic arthritis;
- systemic lupus erythematosus;
- dermatomyositis;
- syphilis;
- sarcoidosis;
- pemphigus.
Figure 8. Trachyonychia in a patient with psoriatic arthritis without skin involvement
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Onychoschizia – A Nail Stratification
The most common cause is trauma, but nail delamination is also seen with:
- anomalies in the development of cartilaginous and bone tissues;
- true polycythemia – a disease associated with an increase in the number of red blood cells and the risk of blood clots;
- systemic therapy with retinoids.
Color Anomalies
White spots on the nails are called leukonychia
Leukonychia is of three types:
- True – associated with violations of the matrix, manifested in the nail plate;
- Apparent – related to breaches of the nail bed.
- Pseudo – associated with external factors, such as fungal diseases.
Figure 9. White spots on the nails with a fungal infection
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
In systemic diseases, leukonychia is usually true or apparent.
Mees’ lines are true leukonychia, which appears as one or more narrow white lines running across the nail parallel to the lunula. Mies’ lines do not disappear with pressure and eventually move towards the tip of the nail. Among the reasons:
- arsenic poisoning;
- Hodgkin’s lymphoma, leprosy, tuberculosis, malaria, shingles;
- chemotherapy, carbon monoxide poisoning, and antimony;
- renal and heart failure, pneumonia, childbirth.
Muehrcke’s lines are imaginary leukonychia, characterized by a double white transverse stripe. A possible cause is swelling of the nail bed, which puts pressure on the vascular bed. Muercke’s lines are characteristic of hypoalbuminemia and disappear when the protein level is normalized. Mürke lines are also observed at:
- nephrotic syndrome;
- glomerulonephritis;
- liver diseases;
- chemotherapy;
- malnutrition.
Figure 10. Muehrcke lines in a patient with an end-stage renal disease with hypoalbuminemia <2 gm%
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Half-white nails (Lindsey’s nails) – sham leukonychia, seen in patients with chronic kidney disease with uremia.
Figure 11. Lindsey’s nails in a patient with chronic kidney disease
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Terry’s nails are sham leukonychia, white on the cuticle and standard on the tip. Terry’s nails are associated with the following:
- congestive heart failure;
- diabetes mellitus in adults;
- diseases of peripheral vessels;
- hemodialysis;
- HIV.
Figure 12. Terry’s nails in a patient with congestive heart failure
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
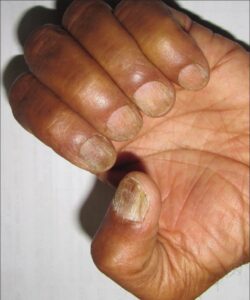
Melanonychia – Brown Spots on the Nails
Brownish-black nail pigmentation is usually associated with lichen planus but can also be related to racial pigmentation. Sometimes melanonychia is observed with:
- malignant melanoma;
- taking medications: antimalarials, minocycline, phenytoin, psoralens, sulfonamides, zidovudine, doxorubicin, methotrexate, azathioprine;
- hemochromatosis – iron overload;
- malnutrition;
- diseases of the thyroid gland;
- smoking;
- HIV infection;
- Addison’s disease – chronic insufficiency of the adrenal cortex.
Figure 13. Brown spots on nails in a patient with HIV
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Blue or Purple Nails – Cyanosis
Cyanosis appears as a result of low tissue oxygen saturation and is of two types:
- Congenital heart defects cause central cyanosis, manifested as a bluish tinge of the mucous membrane and extremities.
- Peripheral cyanosis is caused by vasoconstriction and decreased peripheral blood flow, manifested as blue nails. It is associated with exposure to cold, congestive heart failure, and peripheral vascular disease.
Yellow Nails
The yellowish coloration of the nails and mucous membranes results from the deposition of bilirubin and can manifest severe liver disease or the destruction of red blood cells.
Nicotine nail coloring. Smokers’ nails turn yellow due to nicotine deposits. Yellowing of the nails may indicate the risk of developing smoking-related diseases, including:
- lung carcinoma;
- chronic obstructive pulmonary disease;
- cardiac ischemia.
Yellow nail syndrome is characterized by thickening and staining of the nails in yellow or yellow-green color. The lunula is dark, and the nails’ transverse and longitudinal curvature is increased with cuticle loss. The syndrome is often associated with systemic disease, most commonly lymphedema, and impaired breathing due to pleural effusion.
Figure 14. Yellow nail syndrome
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Shrapnel Hemorrhages under the Nails
Shrapnel hemorrhages look like splinters. The simultaneous appearance of bruising under several nails indicates a systemic cause. Shrapnel hemorrhages usually occur with the following:
- psoriasis;
- infective endocarditis;
- rheumatic heart disease;
- replacement of heart valves;
- systemic lupus erythematosus;
- antiphospholipid syndrome;
- intravenous drug addiction;
- congenital heart defects.
Figure 15. Shrapnel hemorrhage in bacterial endocarditis
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Red Lunula
The red lunula can merge with the color of the rest of the nail, or a pale line can separate it. The lunula becomes invisible when pressed on the nail. Lunula turns red when:
- collagen vascular diseases;
- heart failure;
- chronic obstructive pulmonary disease;
- cirrhosis of the liver;
- chronic urticaria;
- psoriasis;
- carbon monoxide poisoning.
Telangiectasia – Vascular Asterisks of the Nail Bed
Periungual telangiectasia can be a manifestation of:
- systemic sclerosis;
- systemic lupus erythematosus;
- dermatomyositis;
- diabetes;
- chronic obstructive pulmonary disease;
- rheumatoid arthritis.
Figure 16. Telangiectasia of the nail bed in a patient with systemic lupus erythematosus
Image source: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4375768/
Nail Abnormalities in Organs
| Organ system/diseases | Nail changes |
| Excretory | Half-white nails, Muercke’s lines, Terry’s nails, splinter hemorrhages, Mies’ lines |
| Respiratory | Yellow Nail Syndrome |
| Digestive | Terry’s nails, azure lunula, Muercke’s lines, brittle nails, longitudinal grooves, leukonychia vera (white patches) |
| Cardiovascular | Shrapnel hemorrhages, concave nails, red lunula, prolapsed nails |
| Hematopoietic | Hemorrhages, gray or blue nails, leukonychia |
| Endocrine | Longitudinal pigmented band, short and brittle nails, periungual erythema and telangiectasia, detachment of the nail from the nail bed |
| Central nervous | Lesch-Nyhan syndrome, Beau’s lines |
| Infectious diseases | Inflammation of the periungual fold, detachment of the nail from the cuticle, brittle nails, subungual abscess |
| Psychiatric disorders | Obsessive habit of damaging one’s nails, white streaks on the nails |
| Systemic lupus erythematosus, systemic sclerosis, rheumatoid arthritis, dermatomyositis | Beau’s lines, periungual telangiectasia, splinter hemorrhages, torn cuticles, scars |
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
Nail as a window of systemic diseases