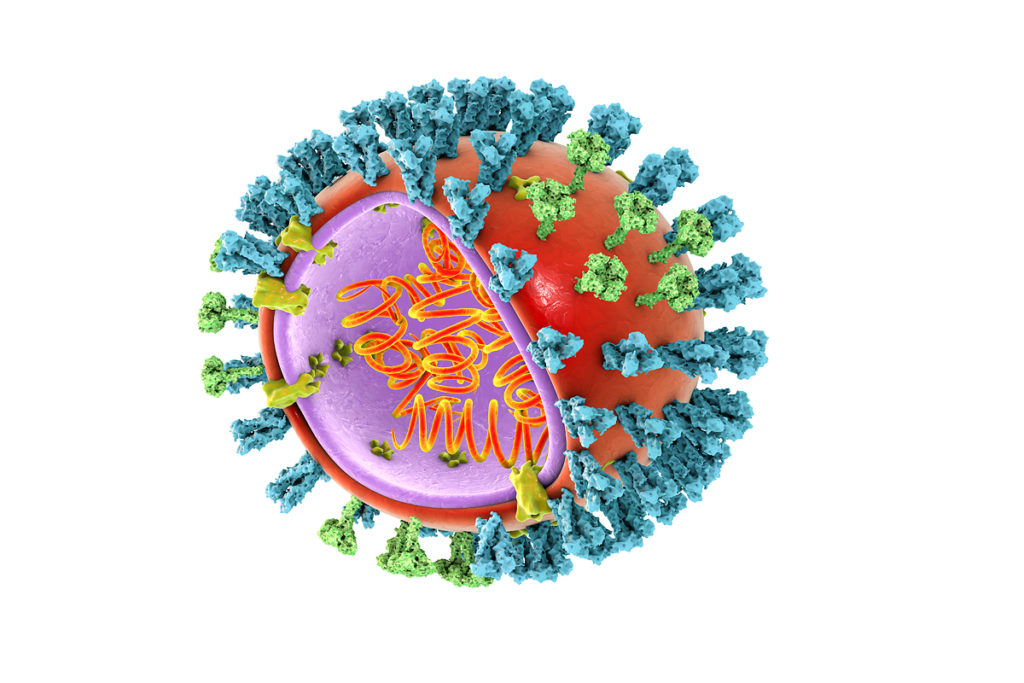
Coronaviridae is a family of single-stranded RNA viruses that can infect most species of domestic and wild animals, as well as humans. As a rule, human infection with coronaviruses leads to mild symptoms from the respiratory tract. Coronaviruses are one of the leading causes of the common cold. However, over the past 18 years, we have witnessed the emergence of highly pathogenic human coronaviruses, including SARS-CoV-1 SARS, MERS-CoV Middle East respiratory syndrome, and the new SARS-CoV-2.
Although SARS-CoV-2 primarily hits lung epithelial cells and causes respiratory infection, there is growing evidence that intestinal epithelium may also be infected. Numerous studies report gastrointestinal symptoms, such as diarrhoea at the beginning of the disease, and reveal the prolonged release of a large number of coronavirus genomes in the faeces. It happens even the virus is absent in oropharyngeal smears. To date, it remains unknown whether there is a possibility of faecal transmission of SARS-CoV-2, but health institutions around the world emphasize this possibility.
The presence of a large number of coronavirus genomes in the faeces hardly explains by swallowing the virus that multiplies in the throat. It is also unlikely that the cause is the loss of barrier function of the intestinal epithelium, which will allow the virus to release genomes inside the body into the lumen of the intestine. Most likely, a large number of coronavirus genomes in the faeces is associated with active replication in the intestinal epithelium.
Many animal coronaviruses are well known as intestinal and transmitting by the faecal-oral route. Previously, it was reported that SARS-CoV-1 and MERS-CoV were present in the gastrointestinal tract of infected patients.
Intestinal biopsy of patients infected with SARS-CoV-2 shows the presence of replicating viruses in the epithelial cells of the small and large intestine. SARS-CoV-2 infection of the gastrointestinal tract is confirmed by the fact that the ACE2 virus receptor is expressing in intestinal epithelial cells. Single-cell sequencing analysis shows that its expression is even higher in intestinal cells than in lung cells.
We have conducted a study to understand how intestinal epithelial cells (IECs) respond to the SARS-CoV-2 virus.
hIECs infection with SARS-CoV-2 virus
First, SARS-CoV-2 (the BavPat1 strain) was propagated in the Vero cell line of a green monkey. To detect viral infection, we use an antibody against the nucleoprotein (N) region, which is conservative between SARS-CoV-1 and SARS-CoV-2. Besides, we used a J2 antibody that detects double-stranded RNA (dsRNA). dsRNA is a hallmark of RNA virus replication. Cells positive for N were always positive for dsRNA. The Vero infected cell supernatants were collected 48 hours after infection (hpi). The number of virus particles present (MOI, a multiplicity of infection which is the ratio of the number of viral particles to the number of target cells) was measured using the TCID50 approach for Vero cells.
Then, T84 and Caco-2 cell lines derived from colon cancer infected SARS-CoV-2 at MOI 0.5 (as determined in Vero cells). These cells expressed both ACE2 and TMPRSS2. At different periods after being infected, T84 and Caco-2 cells were fixed and stained with anti-N and anti-dsRNA antibodies.
The results show that CACO-2 cells infected with SARS-CoV-2 are detecting after four hpi, and after 24 hpi, the infection has interfered into most of the cells. Similar results are observing in T84 cells, but infection detection was slightly delayed compared to Caco-2 cells. Although the same amount of SARS-CoV-2 is using to infect cells, only 20% of the cells are infected after 24 hpi.
These observations are consistent with an increased viral genomes number, and the virus particles release into infected T84 and Caco-2 cells.
Infection of human intestinal epithelial cells (hIECs) with SARS-CoV-2 is associated with the generation of an IFN-mediated immune response. Simultaneously with the differences between T84 and Caco-2 cells observed in de novo virus replication and production, T84 cells showed a much more robust immune response than Caco-2 cells. However, far fewer T84 cells were infected. The level of the protein secreted by a type I IFN was below the detection limit.
These results show that IECs infect easily with SARS-CoV-2 and that infection of Caco-2 cells results in a weaker innate immune response, which is associated with higher infectious production of the de novo virus compared to T84 cells. This observation suggests that an IFN-mediated immune response controls SARS-CoV-2 infection in intestinal epithelial cells.
IFN prevents infection of intestinal epithelial cells SARS-CoV-2
To determine the function of IFN in limiting SARS-CoV-2 replication and de novo virus production in human IEC, T84 and Caco-2 cells were subjected to dummy pretreatment of type I IFN (IFN-β1) or type III IFN (IFN-λ). 24 hours later, the cells were infected with SARS-CoV-2 at a MOI of 0.5 (as determined in Vero cells) in the presence or absence of IFN. After 24 hpi, the cells were stained using antibodies against both N and dsRNA.
The results show that pretreatment of cells with any of the IFN significantly affected SARS-CoV-2 infection of both T84 and Caco-2 cells. A decrease in the number of infected SARS-CoV-2 cells pretreated with one of the IFNS was associated with inhibition of an increased number of the viral genome and a significant decrease in the release of infectious de novo virus particles. These results show that both IFN-β1 and IFN-λ can effectively prevent infection of SARS-CoV-2 intestinal epithelial cells. It indicates that an IFN-mediated immune response can control SARS-CoV-2 infection in human IEC.
IFN-mediated immune response controls SARS-CoV-2 infection in HIEC
To determine whether endogenous IEC generated IFN levels control SARS-CoV-2 replication and de novo virus production, we used IECS devoid of type I IFN receptor (IFNAR1; AR – / – ) or type III IFN receptor (IFNLR1; LR – / – ) or depleted by both IFN receptors (double knockout [dKO]). To control that the cells were knockout at the type I IFN receptor (AR -/ -) and/or type III IFN receptor (LR -/ -), T84 cells were treated with either IFN or IFN-stimulated gene (ISG) production of IFIT1. Knockout cells of the type I IFN receptor (AR – / -) responded only to IFN-λ, whereas cells knockout at the type III IFN receptor (LR -/ -) responded only to IFN-β1. The dKO cells of the IFN receptor did not respond to any of the IFNs.
Wild-type T84 cells (WT) and IFN Knockout T84 cells have infected SARS-CoV-2 at MOI 0.1 (as determined in T84 cells). After 24 hpi, the cells were immuno-coloured using an anti-N antibody, and the number of infected cells was determined using fluorescence microscopy.
The results showed that depletion of the type I IFN receptor (AR -/ -) resulted in a slight increase in the number of infected cells. Moreover, depletion of the type III IFN receptor (LR -/ -) led to a seven-fold increase in the number of infected cells. Similar results appeared when IFN receptors of both types (I and III) were depleted (dKO).
An increase in the number of infected cells with depletion of the type III IFN receptor (LR -/ -) was associated with a significant increase in the number of copies of the viral genome and with an increase in de novo virus production by three orders of magnitude.
Together, these results suggest that the immune response mediated by type III IFN is actively involved in controlling SARS-CoV-2 infection in human IECs.
To uniquely assess the importance of an IFN-mediated antiviral response, a pan-JAK inhibitor (pyridone-6) was used to inhibit activation of STAT1 phosphorylation and block ISG production. Treatment of T84 cells with a pan-JAK inhibitor completely inhibits the signal transmission of both type I and type III IFN receptors.
T84 cells treated with imitation and pretreated with pyridone-6 were infected with SARS-CoV-2 for 24 hours and analyzed by fluorescence microscopy after immunostaining using an anti-n antibody.
The results show both a significant increase in the number of infected cells and an increase in the number of copies of the viral genome in cells treated with the pan-JAK inhibitor.
According to results obtained in type III IFN receptor-depleted cells, this increase in the number of infected cells is also associates with an increase in the production of infectious de novo virus particles. These results support a model in which an IFN III-mediated immune response controls SARS-CoV-2 infection in hIECs.
Primary human intestinal organoids support SARS-CoV-2 infection, replication, and de novo virus formation
Organoids obtained from the human colon from two different donors were used to find out whether primary hIEC can become infected with SARS-CoV-2 and support de novo virus production.
Entire ultrastructural organization and differentiation of cell types (enterocytes, goblet cells, enteroendocrine cells, stem cells) were confirmed by confocal fluorescence microscopy and qRT-PCR against cell-specific transcripts. Previously established protocols were used to differentiate and infect human intestinal organoids with viruses.
Undifferentiated organoids are seeding on iBIDI cells coated with human collagen. 24-hours after seeding, differentiation was induced by removing Wnt3a and reducing the amount of R-spondin and Noggin for four days. After complete differentiation, the organoids are infecting with SARS-CoV-2. After 24 hpi, we analyzed the infection using immuno-staining using anti-N and anti-dsRNA antibodies and using qRT-PCR.
The results show that colon organoids were infected with SARS-CoV-2 regardless of the donor. It is noted by the presence of cells positive for both N and dsRNA. The quantitative evaluation showed that 8-13% of cells infecting in each donor. Infection was associated with an increase in the number of copies of the viral genome.
Infection of organoids did not lead to the production of type I IFN (IFN-β1) but led to robust activation of type III IFN (IFN-λ).
The lack of production of type I IFN may be due to the kinetic delay in the production of type I IFN compared to type III IFN, but this needs careful double-check in further experiments. Another possibility is that SARS-CoV-2 encodes a specific antagonist that only counteracts the production of type I IFN. However, further research is needed to prove this concept.
To determine whether exogenously added IFNS could prevent SARS-CoV-2 infection, colon organoids were treated fictitiously or pretreated with IFN-β1 and IFN-λ, and then infected with SARS-CoV-2 for 24 hours.
The results show that pretreatment of colon organoids with both IFN-β1 and IFN-λ significantly weakens infection. This effect was associated with a decrease of the SARS-CoV-2 genome and a decrease of infectious de novo virus particles.
Overall, these results show that human colon organoids can support SARS-CoV-2 infection, replication, and de novo virus formation. The immune response mediated by type III IFN plays a critical role in controlling virus replication.
The research is granted by the Chica and Heinz Schaller Foundation and the Deutsche Forschungsgemeinschaft (DFG) project.
The reaction of intestinal and lung epithelial cells to SARS-CoV -2
It is well known that intestinal epithelial cells in vivo are less immunoreactive due to the intestinal microenvironment (microbiota and tissue-specific immune cells). Therefore, it is likely that the IEC will demonstrate a severely weakened immune response, allowing for even greater replication of SARS-CoV-2.
Caco-2 are excellent culture models supporting both SARS-CoV-2 and SARS-CoV-1. The study highlights the potentially crucial role of intestinal epithelial cells in the prognosis of patients with COVID-19.
Interestingly, infection with SARS-CoV-2 in human lung epithelial cells Calu-3 also triggers an immune response. Whereas in A549 cells (lung adenocarcinoma cells), in ferret models and human lung tissues, infection with SARS-CoV-2 results in a limited and muted immune response that does not induce type IFN I and type III.
The reason for differences in the amount of IFN in lung and intestinal epithelial cell infection is currently unclear. Like intestinal epithelial cells, lung epithelial cells usually have a high immune response and produce interferons during viral infection. The absence of IFN in lung epithelial cells after infection with SARS-CoV-2 may be specific to this virus in this tissue.
Compared to airway epithelium, intestinal epithelium elicits a typical antiviral response. It means that the host-pathogen interaction should be considered in a tissue-specific manner, since the establishment of the different cellular responses and antiviral measures for the lungs, intestines, and other organs.
Conclusions
Characterization of the intestinal life cycle of SARS-CoV-2 is necessary to determine whether the viral infection observed in the intestine is a result of faecal/oral transmission or a manifestation of the spread of the virus from the lung to the intestine.
The results of the study suggest that at the beginning of infection with SARS-CoV-2 hIEC, an antiviral response will occur via the type III IFN signalling pathway. Since immune cells are involved in the formation of an innate immune response, type I IFN will be secreted from these cells and can affect intestinal epithelial cells, further enhancing their antiviral action against SARS-CoV-2.
As for severe pulmonary cytokine storm-based pathologies, the findings that lung epithelial cells cause a muted immune response to SARS-CoV-2 infection may show that cytokines come from an alternative source. The source may be from local immune cells or the gastrointestinal mucosa, given the robust immune response generated by primary hIECs. Many cytokines are released from epithelial cells in the direction of lamina propria and quickly enter the blood circulation, potentially contributing to inflammation and pulmonary pathology.
To effectively fight a pandemic, you need to assess the complexity of the disease entirely. This requires the virus life cycle and its interaction with the host to characterize for each site of infection: both for the lungs and the intestines.
hIECs are a productive site of SARS-CoV-2 replication, and this may be crucial for the study of SARS-CoV-2 infection and pathologies observed in patients with COVID-19. The results of the study highlight the crucial role of type III IFN in limiting SARS-CoV-2 in the intestinal epithelium.