Inflammation is the natural response of the immune system to pathogens. This reaction is provided by cytokines to protect the body. In some cases, the immune system is hyperactive and causes cytokine release syndrome.
Cytokine release syndrome (CRS) is a life-threatening systemic inflammation. It occurs as a complication from drug immunotherapy for cancer and autoimmune diseases, as well as a reaction of the immune system to severe viral infections. Symptoms of CRS include fever, headache, muscle and joint pain, fatigue, rash, nausea, and hypotension. The symptoms of CRS are increasing gradually after immunotherapy. If symptoms worsen quickly, CRS is called a cytokine storm. CRS can lead to cardiovascular collapse, multiple organ failure, and death.
The occurrence of CRS after immunotherapy creates a problem in specific drug intakes, such as oncolytic viruses and bacteria, recombinant lymphokines, natural and bispecific antibodies, and T-cells that destroy cancer cells.
Cancer treatment with ANP-Clostridium novyi-NT bacteria
A growing tumor lacks blood supply, and its tissues experience hypoxia. Hypoxia suppresses the immune system’s antitumor response. Due to a lack of oxygen, tumor cells change their metabolism. That makes them resistant to many medications.
Scientists have studied the treatment of cancer using anaerobic spore-forming bacteria Clostridium novyi-NT. C.novyi-NT spores develop only in hypoxic tumor tissues and can destroy them.
But when mice were injected with large doses into extensive tumors, there was not only tumor lysis, but also sepsis with a steady release of cytokines caused by a bacterial infection. Sepsis could not be extinguished with the antibiotic metronidazole, and the mice died.
Even when the mice were treated with anti-inflammatory drugs before treatment: dexamethasone and antibodies against TNF, Il-6 receptor (IL-6R), and IL-3, only IL-6R blockade gave improvement. But this did not affect the survival rate.
Scientists changed the genome of C.novyi-NT by adding the function of high expression of atrial natriuretic peptide (ANP). ANP is a peptide hormone that hearT-cells secrete to regulate water-electrolyte homeostasis. ANP reduces the release of cytokines and has anti-inflammatory properties, while not suppressing tumor lysis. The new genome was named ANP-C.novyi-NT.
The introduction of ANP-C.novyi-NT into subcutaneously implanted CT26 tumors resulted in the growth and reduction of the tumor. In mice that were injected with ANP-C.novyi-NT, plasma levels of ANP and cyclic GMP were 2-4 times higher than in mice that were injected with C.novyi-NT. Tumor germination was equally effective in both strains. But more than 80% of the mice injected with ANP-C.novyi-NT survived, and 84% of the tumor completely collapsed. In the case of the introduction of C.novyi -NT has not endured any mouse.
In mice that were injected with ANP-C.novyi-NT, inflammation, and tissue damage were less than in mice that were injected with C.novyi-NT. There were fewer infiltrating CD11b +myeloid cells in the liver, spleen, and lungs. Levels of cytokines of myeloid origin (IL-1β, IL-6, MIP-2), chemoattractants (KC), and TNF and IFN-γ were significantly lower. Also, the mice that were injected with C.novyi-NT had increased lung permeability, and myeloid bone marrow hyperplasia was present.
Catecholamines are control molecules, including epinephrine, norepinephrine, and dopamine.
In mice treated with ANP-C.novyi-NT, reduced inflammation was accompanied by noticeably lower levels of circulating catecholamines. The ratio of plasma volume to red blood cell volume was the same in both groups of mice. It shows that lower levels of circulating catecholamines were not associated with changes in volumetric homeostasis.
Osmotic pumps are subcutaneously implanting in mice before treatment with C.novyi-NT to confirm the protective effect of ANP. 75% of the mice survived, and 77% of the tumor completely collapsed. In 23%, the response to therapy was stable but did not lead to a cure. Systemically administered ANP, as well as ANP – C.novyi-NT, reduced the level of Pro-inflammatory cytokines, catecholamines, and tissue damage.
What catecholamine increases inflammation?
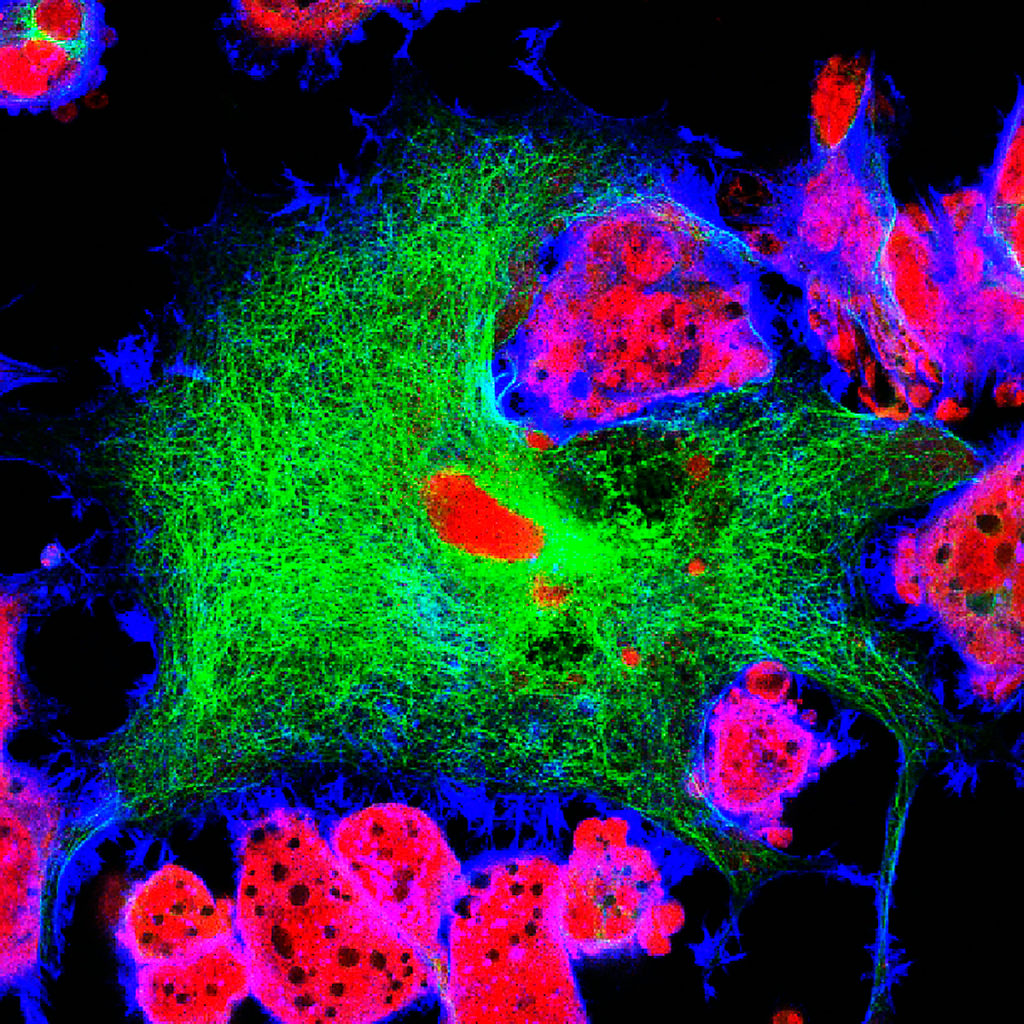
Macrophages are cells of the immune system that digest foreign particles, bacteria, remnants of dead cells, and cancer cells. Macrophages are the primary source of inflammatory cytokines. Macrophages detect external elements in the body and secrete catecholamines, and react to catecholamines by increasing the production of cytokines.
The release of cytokines was observed in mice after administration of lipopolysaccharide (LPS). Mice receiving LPS were subcutaneously implanted with osmotic pumps that release epinephrine, norepinephrine, and dopamine. Exacerbation of inflammation and high mortality rates were observed only in LPS-treated mice with epinephrine osmotic pumps. These mice had higher levels of IL-6, TNF, and KC than mice that received only LPS or only epinephrine, although all of them had higher levels of cytokines.
How does ANP affect catecholamine synthesis?
Catecholamine synthesis under the influence of ANP was studied in mice in stimulated peritoneal macrophages. The mice were injected with LPS. ANP reduced catecholamine production. Levels of IL-6, TNF, MIP-2, and KC also decreased. LPS, combined with epinephrine, increased inflammation. ANP also reduced this increased inflammatory response.
Catecholamines are synthesized in the following order: tyrosine, L-DOPA, dopamine, norepinephrine, and epinephrine. Tyrosine hydroxylase (TH gene) is necessary for the first stage of catecholamine synthesis.
α-methylthyrosine (MTR) blocks TH and the conversion of tyrosine to L-DOPA, which suppresses the synthesis of catecholamines. MTR reduces the levels of catecholamines that are produced by stimulated macrophages. Also, under the influence of MTR, the levels of cytokines that release macrophages are reduced. The results of these studies on mice were confirmed in studies on human macrophages.
Macrophage catecholamines cause an inflammatory response
The study used mice without the TH gene in peritoneal macrophages. When LPS and epinephrine stimulated these macrophages, the production of catecholamines and cytokines was reduced. It confirms that the autocrine production of catecholamines increases the inflammatory response of macrophages. Interestingly, impaired catecholamine production reduced cytokine release and mortality in mice without the TH gene in macrophages.
MTR in vivo reduces catecholamine and cytokine levels
Before the introduction of LPS, the mice were given MTR. 75% of the mice survived. While in the control group without MTR, only 10% of the mice left alive. MTR steadily reduced catecholamine and cytokine levels and mortality. The effect of MTR was dose-dependent. A similar result was observed in mice injected with LPS when α1-adrenoreceptors were blocked. These receptors respond to norepinephrine.
MTR and bacterial infection-induced cytokine release syndrome
Treatment of tumors with C.novyi-NT bacteria causes cytokine release syndrome and increased mortality in mice. Before the introduction of C.novyi-NT, MTR was administered to mice. MTR reduced catecholamine and cytokine levels and significantly reduced mortality. 85% of the mice survived, compared to 8% in the control group.
C.novyi-NT gram-positive bacteria. Gram-negative bacteria are also used in experimental cancer treatments. Gram-negative bacteria also cause sepsis, but it is different from the sepsis caused by C.novyi-NT.
Scientists have investigated how MTR affects mortality from sepsis when treated with gram-negative bacteria. The study was performed on a mouse model of caecal ligation and puncture. MTR was reducing catecholamine, cytokine levels and mortality. 22% of the mice survived the acute phase, but all the mice in the control group have died. MTR, in combination with the β-lactam antibiotic imipenem, improved the result: 67% of the mice have survived. In the group that received only imipenem, only 10% have survived. This result shows that mortality is affected by both bacterial infections and the body’s response – cytokine release syndrome.
MTR and cytokine release syndrome caused by T-cell activators
After treatment with non-bacterial drugs that activate T-cells, cytokines are also released. This effect is essential for transplantation. For example, antibodies against CD3 t-cell molecules block t-cell receptors. This treatment weakens autoimmunity and reduces the risk of allograft rejection, but causes T-cell activation and cytokine release syndrome.
The researchers examined the impact of MTR on mortality after the application of antibodies to CD3. Immunodeficient BALB/c mice aged 5-6 months were used for the study. CD3 caused the release of cytokines and increased levels of catecholamines. Pre-administration of MTR reduced the levels of catecholamines and cytokines IL-6, TNF, MIP-2, and KC. The levels of cytokines IL-2 and IFN-γ did not change. Reduced MTR was associated with the release of cytokines mortality. Similar results were observed in mice with the absence of the TH gene in macrophages. These mice did not increase levels of catecholamines and cytokines, which confirms that myeloid cell catecholamines play an essential role in CRS management.
Cytokine release syndrome in treatment with CART-cells
Genetically engineered T-cells CART are also used to treat cancer. On the surface of these cells, receptors are constructed that allow T-cells to recognize and attach to a specific antigen on tumor cells. These receptors are called chimeric antigen receptors or CAR. The CART-cells introduced to the patient multiply, recognize and kill cancer cells that carry the antigen on their surface.
Treatment with CART-cells often causes CRS. An IL-6R and IL-1R block is used to suppress CRS.
Scientists investigated in vitro whether CART expressed an increased amount of catecholamines when interacting with tumor cells. CD19+ Raji tumor cells derived from human Burkitt lymphoma were used for the study. As a treatment, hCART19 cells directed against CD19 are using. Interaction of Raji cells with hCART19 cells caused the release of catecholamines and cytokines IL-2, TNF, IFN-γ, MIP-1α. Both MTR and ANP weakened this effect.
When epinephrine was added to co-cultured Raji and hCART19 cells, increased expression of catecholamines and cytokines was observed. The introduction of the protein synthesis inhibitor cycloheximide (CHX) suppressed this effect. This result shows the need for de novo protein synthesis.
Scientists have investigated the role of catecholamines in CRS in vivo in the treatment of CART19. The study used adult transgenic NSGS mice that Express human myeloid cytokines IL-3, GM-CSF, and SCF and model human CRS. The mice were given a sublethal dose of Raji cells and hCART19 cells. The mice were divided into two groups.
In the first group, hCART19 was administered at half the time of average survival in untreated mice. It has created a high risk of CRS due to increased tumor load. All the mice in the first group died because hCART19 cells cannot save mice with a high tumor load. At the time of death, the mice in the first group had excessive levels of catecholamines and cytokines originating from human T-cells (Hs IL-2, Hs IFN-γ and Hs TNF) and mouse cells (Mm IL-6, Mm KC and Mm MIP-2). Pretreatment of MTR significantly reduced the levels of circulating catecholamines in both human and mouse cytokines, but the mice still died from the progressive disease.
The second group was given hCART19 after a third of the average survival time. In this case, the tumor load is low, and it is possible to evaluate the antitumor response. HCART19 cells destroyed the tumor, mostly in mice pre-treated with MTR. MTR significantly reduced the levels of catecholamines and cytokines Hs TNF, Mm IL-6 and Mm KC, and less for Hs IFN-γ and Hs IL-2. ANP gave similar results. Neither MTR nor ANP prevented hCART19 from multiplying and destroying the tumor. They both effectively prevented CRS.
In mice that were injected with the same amount of nontransduced T-cells (UT-T), catecholamine, cytokine levels, and survival rates did not change.
MTR and ANP effects were tested on a syngeneic mouse model. Mice were injected with mouse leukemia cells. The mice were then treated with mCART19 cells against mouse CD19. The pretreatment of MTR and ANP did not reduce the effect of mCART19 but reduced the systemic level of catecholamines and cytokines. This result confirms that MTR and ANP can prevent CRS while maintaining antitumor effectiveness.
Catecholamines increase inflammatory damage caused by bacterial and non-bacterial causes. It caused be self-reinforcing catecholamine loop of direct communication in myeloid cells. It is possible that T-cells and adrenal cells, which also produce catecholamines, are also involved in this process. For the synthesis of catecholamines, the TH gene is needed. α1-adrenoreceptors of immune cells react to catecholamines. MTR and the α1-blocker prazosin can be used to break this chain and reduce the inflammatory response. The FDA approves both drugs for the treatment of hypertension. Therefore, their use is possible in clinical trials of drugs whose use is limited by the risk of CRS.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary: