In 1957, antiviral defence proteins – interferons (IFN) were discovered. Type I IFNS (IFNα/β) stimulate the expression of ISG (interferon-stimulated genes). ISG protein products fight viruses in infected and neighbouring cells. Interferons have two ways to fight the infection. They can affect the life cycle of the virus, or they can disrupt the cell’s metabolism and inhibit the translation mechanism.
Pathogens or host genetic properties can cause excessive IFN production. It can provoke severe diseases. That is going with flu, tuberculosis, lupus, HIV, and Aicardi-Gutierrez syndrome.
Excessive IFNα/β signalling can cause tissue damage and immune paralysis — a condition in which the immune response is absent. The body can regulate the level of IFNα/β signals to avoid the damage.
An organism regulates the level of interferon signals
Ubiquitin is a protein that is synthesized in all cells containing the nucleus (eukaryotic). Ubiquitin regulates the degradation of other proteins inside the cell. It also regulates the activity of signalling pathways and affects the transmission of signals to the cell nucleus. The addition of ubiquitin to the target protein is called ubiquitination.
Each type of IFN interacts with its related receptor. The receptor is a cell surface type I IFN — IFNAR. It consists of two chains: IFNAR1 and IFNAR2.
After transmitting the interferon signal, IFNAR1 is ubiquitinated. That is resulting in the temporary suppression of interferon receptors, which limits further IFN responses. The described mechanism protects the body from inflammatory processes.
The study: how does temporary suppression of IFNAR1 affect the redundant IFN signal
Priming – a preparation of cells for the subsequent response to stimulation.
A naive cell is a mature cell that can perform the full range of its functions but has not yet been stimulated to respond to a specific antigen.
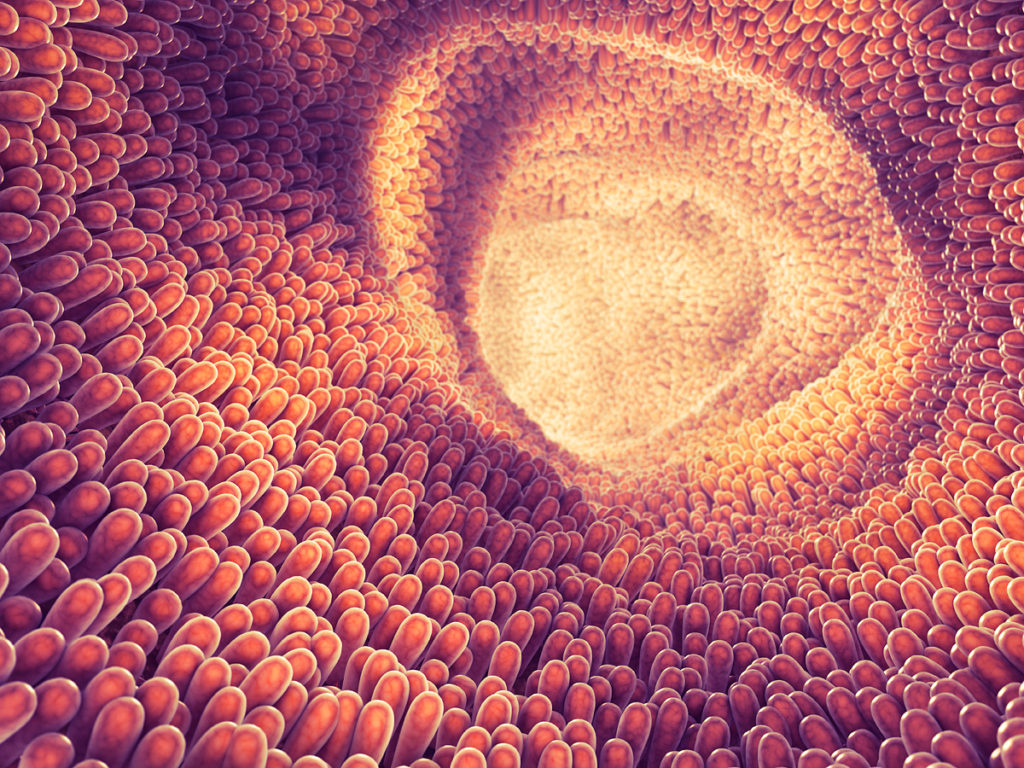
The intestinal microbiota is a community of commensal, symbiotic, and pathogenic microorganisms that live in the gut. The microbiota is crucial for the host’s immunological, hormonal, and metabolic homeostasis.
Tonic signals are signals caused by always present triggers.
To understand how temporary suppression of IFNAR1 affects the excess IFNα/β signal, a study was conducted on mice that are unable to ubiquitinate IFNAR1 after transmission of the interferon signal (IFNAR1SA mice). In these mice, the interferon receptor is not suppressed, and the IFN signal is amplified. IFNAR1SA mice have elevated baseline ISG levels.
The study showed that:
- To fine-tune the degree of priming of IFNα/β in naive lung cells, the regulation of surface levels of IFNAR1 is essential.
- Because of the increased baseline ISG, IFNAR1SA mice are more resistant to influenza infection.
- In both IFNAR1SA and wild-type (WT) mice, the microbiota enhances interferon-controlled ISG expression. To a greater extent, this occurs in epithelial cells.
IFN tonic signals determine the strength of infection-induced IFNα/β signals and form the resistance of epithelial cells to viral infection.
IFNAR1-dependent signals control the ISG signature in pulmonary stromal and hematopoietic cells
A signature is a single or combined group of genes in a cell with a unique characteristic expression pattern.
CD45 is a marker of hematopoietic cells.
It has been suggested that in uninfected animals, Ifnß tonic signals lead to initial activation of the IFN pathway.
To find out whether this works for both hematopoietic and or stromal cells, measured ISG levels in CD45-positive and CD45-negative lung cells. The study used C57BL/6 mice — the most popular type of laboratory mice. During the investigation, two doses of antibody aIFNAR1 (MAR1) were administered at 48-hour intervals. Two days after the second injection, both groups of cells demonstrated that the interferon-stimulated Rsad2 and Oasl2 genes were suppressed after treatment. This result shows that IFN tonic signals control the initial ISG level in both hematopoietic and stromal cells.
Mice with IFNAR1 deficiency (IFNAR1– / –) had lower levels of ISG expression in both cell groups. These mice do not transmit IFNα/β signals. This result means that in both hematopoietic and stromal cells, IFNAR1-dependent signals control steady-state ISG levels.
IFNAR1 levels control primary ISG expression and interferon-induced immune responses
IFNAR1-dependent signals support the necessary isg1 signature. Setting IFNAR1 levels is a way to control the value of the IFN signal.
To confirm this, IFNAR1SA mice were used that were not able to disable the IFN signal. To verify that IFNAR1SA mice did not have IFNAR1 suppression, bone marrow-derived macrophages (BMDM) processed IFNα4. In BMDM cells of mice IFNAR1+ / + C57BL/6, surface expression of IFNAR1 decreased depending on the dose. In BMDM IFNAR1SA mice, IFNAR1 expression was maintained at a constant level for lower IFNα4 concentrations.
According to the results of fluorescence-activated cell sorting (FACS) analysis, IFNAR1sa naive lung cells had increased initial levels of IFNAR1SA expression in both CD45+ immune cells and CD45-epithelial and endothelial cells. It means that the constant suppression of IFNAR1 leads to the establishment of a physiological surface level of IFNAR1.
In the lungs of IFNAR1SA mice, the established expression of ISG was increased. That demonstrates the surface levels of IFNAR1 control the ISG signature. The IFNAR1 blockade lowered the ISG level. It shows that the ISG signature is in dynamic equilibrium, which requires constant IFN signals to maintain.
The level of ISG was increased in both stromal and hematopoietic cells. In IFNAR1sa lung immune cells, the surface expression of interferon-inducible proteins Sca-1 and PDCA1 was raised, in contrast to C57BL/6 cells.
Together, these results show that surface levels of IFNAR1 control the physiological levels of ISG expression in both stromal and hematopoietic cells. Since the natural activation of the type I IFN pathway is a mechanism for maintaining immune balance in the mucous membranes of uninfected mice, this fact plays a vital role in pulmonary immunity.
Changes in the initial expression of ISG in immune cells were different from changes in the composition of the immune cells of the lungs of IFNAR1SA mice. This fact is consistent with the fact that the structure of immune cells in the lungs of mice IFNAR1– / – is unchanged. It shows the tonic signal of type I IFN supports the signature of IFN in immune cells but does not affect the survival and replenishment of immune cells.
Plasmacytoid dendritic cells (pDC) behave differently. If there is no IFN signal, their number decreases. pDC is supported by type I interferon and is its source.
In previous experiments, WT and IFNAR1SA mice showed ISG expression. To find out if it is caused by interferon originating from pDC, depletion antibodies against the pdca1 plasmacytoid dendritic cell marker were used. PDC depletion did not alter ISG expression in the lungs. It means that other cells are responsible for establishing the initial appearance of ISG in WT and IFNAR1SA mice.
IFNAR1sa mice are more resistant to influenza virus infection
MxA is a restriction factor of the flu virus.
IFNAR1SA MxAtg / tg mice are mice with a transgene encoding human MxA.
How does reduced regulation of IFNAR1 affect the body during influenza virus infection: does it enhance immunopathology or contribute to antiviral protection?
The study found that IFNAR1SA mice are less likely to be infected with the flu virus than WT mice. In IFNAR1SA mice, viral gene expression decreased significantly after 8 hours, and virus replication decreased 2 days after infection.
WT and IFNAR1SA MxAtg / tg mice were infected with the highly virulent PR8 influenza virus. IFNAR1SA MxAtg / tg mice had less weight loss than the WT control group. That confirms the result described above.
What provides antiviral protection in IFNAR1SA mice: baseline ISG levels or increased sensitivity?
16 hours after infection, the viral load decreased in IFNAR1SA lung stromal cells. That is corresponded to higher ISG levels in IFNAR1SA cells compared to WT mouse cells. Later than 16 hours after infection, no further increase in infection-mediated ISG levels was detected in either WT or IFNAR1SA mice. At this early stage of the disease, neither stromal nor immune cells demonstrated interferon mRNA induction. After 8 hours after infection, IFNAR1SA mice decreased their viral load. There was no increase in ISG levels in the stroma or immune cells during this period. These results mean that the early decline in virus replication depends on the initial antivirus state, rather than rapid ISG activation.
48 hours after infection in mice, IFNAR1SA decreased, rather than increased, the level of the IFN protein. The set of immune cells in the lungs did not differ in WT and IFNAR1SA mice. 5 days after infection, Pro-inflammatory cytokines decreased in IFNAR1SA MxAtg / tg mice. These results show that the stable ISG signature in the lung stroma, regulated by interferon, is crucial for early control of the flu virus. The viral load is reduced, and immune responses are reduced.
Also, the reduced immune response is since IFNAR1SA mice are initially less reactive. In vitro, IFNAR1SA respiratory epithelial cells showed higher reactivity to IFNα than WT control cells. In vivo, IFNAR1SA mice attracted immune cells to lungs treated with polyionic acid (used to simulate viral infections) more strongly than the WT control group. This result shows that in IFNAR1SA infected mice, the decrease in the immune response is a result of a reduction in the viral load 8 hours after infection.
The microbiota controls the level of ISG in the epithelium. Therefore, the flu virus is blunted in the early stages of infection. During the first eight hours after infection, virus transcripts are reduced, and viral titers are reduced by more than five times in the first two days. The viral load was decreased early, so anti-inflammatory immune responses were also reduced. It explains the fact that IFNAR1SA mice, which have an increased response to interferon and immune response to stimuli, exhibit a weaker IFN response to the virus than the control group of WT mice.
Increased ISG expression in CD45 cells is crucial for early protection against flu
How do CD45+ and CD45-cells affect the resistance of IFNAR1SA mice to the flu virus?
The study used bone marrow chimaera (BM) from C57BL/6 and IFNAR1SA mice . 6 to 8 weeks after BM recovery, a chimera was infected with the flu. Weight loss in IFNAR1SA chimaeras was significantly lower than in C57BL/6 mice. In C57BL/6 mice that received IFNAR1SA bone marrow, weight loss was significantly higher than in IFNAR1SA. In the early days of viral infection, C57BL/6 mice that received IFNAR1SA bone marrow showed more severe signs of the disease. It indicates that CD45-cells are crucial for early virus suppression.
In the later stages of infection, weight loss in IFNAR1SA mice that received WT BM was more significant than in control group mice that received IFNAR1SA BM.
At different stages of infection, separate cellular compartments are responsible for antiviral protection. Dispersion analysis for the values of relative body weight on days 3 and 9 after being infected showed that the stroma genotype is responsible for the change in body weight on day 3, and the interaction between stroma and BM genotypes on day 9. That means that early antiviral protection requires IFNAR1-controlled signals in CD45 cells. And to provide late protection, IFNAR1-controlled signals in hematopoietic cells are needed.
The microbiota controls the stable ISG signature in the lung stroma but does not affect the ISG signature in immune cells
What is the reason for increased ISG levels in IFNAR1SA mice?
To test the hypothesis that the cause is the unique microflora in the IFNAR1SA mouse colony, WT mice were kept together with IFNAR1SA mice for a month. Neither WT nor IFNAR1SA mice showed any change in ISG expression in lung cells. IFNAR1SA mice maintained elevated ISG levels. It shows the level of ISG is not increased because of the unique microflora.
Mice that received an oral antibiotic are more susceptible to viruses. To test the hypothesis that the microbiota affects ISG expression in the lungs, WT and IFNAR1SA mice were given an antibiotic in drinking water for 4 weeks. The antibiotic caused a decrease in ISG expression in the stromal compartment but did not affect cells of hematopoietic origin.
Microbiota protects the stroma of the lungs from the flu
Does increased ISG expression lead to resistance to viruses?
To test whether the virus replication block relieves the decrease in ISG by antibiotics in IFNAR1SA mice, WT and IFNAR1SA mice were given an antibiotic for 4 weeks. The control group did not receive an antibiotic. After 4 weeks, the mice were infected with the flu virus. IFNAR1SA mice that did not receive the antibiotic were more resistant to the infection than C57BL/6 mice. IFNAR1SA mice treated with the antibiotic were just as susceptible as the WT control group. It looks like microbiota-controlled signals are responsible for the antiviral resistance phenotype in IFNAR1SA mice. Antibiotics did not change the antiviral resistance of WT mice. A possible cause is the absence of the MX1 influenza restriction factor in C57BL/6 mice.
The experiment was repeated on mice that have the functional Mx gene (MxA). This model is more like a human model. In the early stages of infection, antibiotics increased viral gene expression and virus replication in Mx1+ / + mice. It shows that if there is a restriction factor for influenza, then the microbiota affects early viral control.
Antibiotics increased weight loss and mortality in Mx1+ / + mice as well IFNAR1WT, and in mice Mx1+ / + IFNAR1SA. Mx1+ / + mice expressing IFNAR1SA were better protected than WT.
After 16 hours after infection, the viral load in mice that received the antibiotic increased. Antibiotics reduce the antiviral state in the stromal cells of the lungs. The microbiota causes the priming of lung stromal cells with interferon and establishes an antiviral state that leads to the suppression of flu in the early stages.
These facts emphasize that antibiotic treatment should be carried out with caution. If oral antibiotics are misused, they reduce the antiviral resistance of the epithelium, which is why the flu can be more severe.
The intestinal microbiota is responsible for changes in the initial expression of ISG. To confirm this, the mice that took the antibiotic were given a faecal transplant (FT) with control group material. Antibiotics reduced the level of ISG in the stromal cells of the lungs, and FT returned it to physiological values. FT gave the same therapeutic effect in both IFNAR1wt and IFNAR1SA mice.
GSEA analysis of the MsigDB database showed that the IFNα/β signaling pathway in the lung stroma was suppressed in mice taking the antibiotic. Also, among the ten most significant signalling pathways, several were found to be associated with the immune system and interferon. All of these pathways were enhanced by fecal transplant treatment. FT treatment eliminated antibiotic-induced flu sensitivity.
All these results show that the microbiota increases the interferon-controlled antiviral state in the lung stromal cells and increases resistance to the flu virus.
Fine-tune IFNAR1 levels to balance the antiviral and Pro-inflammatory properties of IFN
If an increased surface expression of IFNAR1 raises antiviral protection, why is the IFN system not initially configured for higher levels?
Type I interferons protect the host from viruses. They interact with the interferon receptor (IFNAR1/IFNAR2) and induce signal transmission and gene expression.
Inflammatory stimuli can trigger ubiquitination and suppression of IFNAR1, thereby attenuating the effects of IFN in vitro.
Studies on Ifnar1SA mice have shown that these mice have increased inflammatory conditions.
IFNAR1SA mice are not able to ubiquitinate IFNAR1 after stimulation of the receptor complex. There is no subsequent suppression of IFNAR1, and the IFN signal is amplified.
That makes IFNAR1SA mice very susceptible to numerous inflammatory syndromes, including acute and chronic pancreatitis, as well as autoimmune and toxic hepatitis.
A small increase in the surface expression of IFNAR1 in IFNAR1SA cells leads to a rise in the appearance of interferon-stimulated genes (ISG) in immune cells and the stromal compartment.
The cells of patients with down syndrome carry an additional copy of the IFNAR1/2 genes on chromosome 21. the Cells of these people Express increased surface levels of IFNAR1 and produce increased amounts of Pro-inflammatory cytokines in response to the virus. In the blood of patients with down syndrome, the ISG signature is increased. Changes in the composition of blood proteins in people with down syndrome are similar to changes in type I interferonopathies and other auto-inflammatory diseases.
These facts and studies in IFNAR1SA mice show how critical is fine-tuning of ifnar1 surface levels for balancing the antiviral and Pro-inflammatory properties of the interferon system.