Content
- Interferon Sources in The Skin
- Interferon Protects Healthy Skin from Infections and UV Damage
- Interferon is Involved in Autoimmune Skin Diseases
- Conclusions
- Source
Interferon Sources in The Skin
Interferons (IFN) are signaling proteins that have antiviral and immunomodulatory functions. Interferons regulate the inflammatory process and activate adaptive immunity to form immunological memory.
Almost all cells can produce type I IFN. However, the type of cells that will be the first to produce IFN depends on the context and the disease. In healthy skin cells, interferon-kappa (IFN-I) stimulates keratinocytes. Interferon-kappa is constantly present in the skin at a low level. However, in acute viral infections, the production of type I-III interferons in the skin increases, preventing the replication of the virus. Chronic viral infections, such as the papillomavirus, also lead to a steady rise in the level of interferon in the epidermis, activating inflammation.
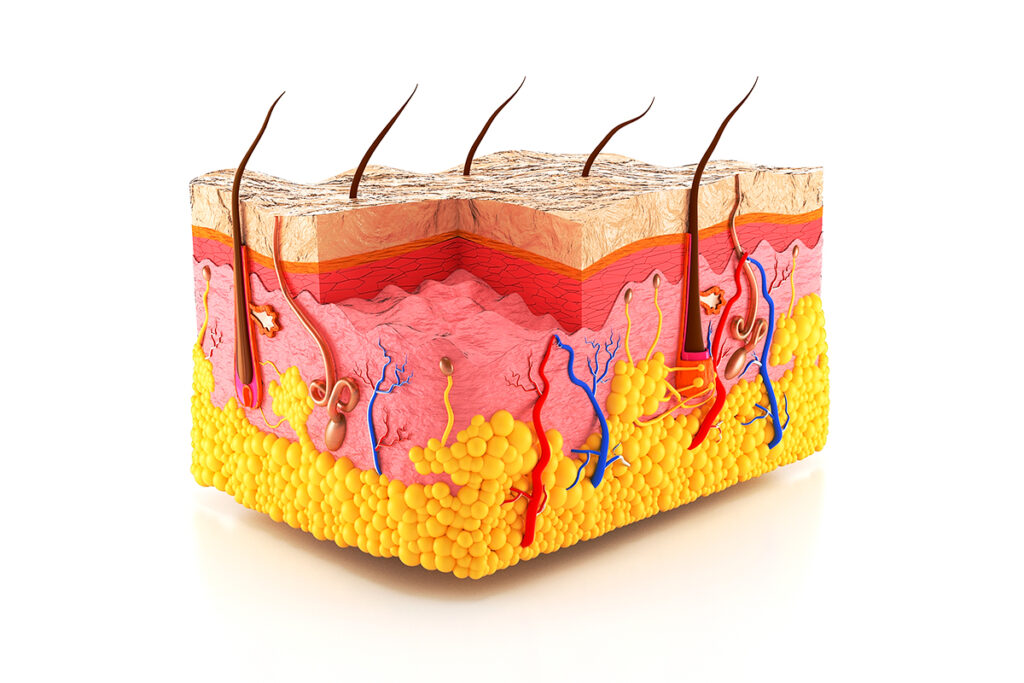
Various autoimmune and inflammatory skin diseases increase the production of IFN-I in the skin. Different interferon-producing cells are attracted to the dermal-epidermal junction during skin infection and inflammation. Among them are plasmacytoid dendritic cells (pDC), Langerhans cells (LC), and monocytes.
Interferon Protects Healthy Skin from Infections and UV Damage
The skin is the main barrier to microbial infections. Keratinocytes – the most numerous skin cells – constantly express IFN-kappa and, in case of disease, can quickly activate the transmission of interferon signals. IFN-kappa can trigger an interferon response in neighboring cells like fibroblasts and dendritic cells and start inflammatory reactions in the skin.
Interferons play a protective and immunomodulatory role in the skin. In normal skin, interferon protects against inflammation caused by UV-B radiation. In studies on mice, type I interferon stimulated the repair of DNA damage caused by ultraviolet B radiation and prevented non-melanoma skin cancer. The study details are placed in the article “Type I Interferons Prevent UV-Induced Skin Cancer“. The study is published in the International Journal of Molecular Sciences.
Interferons are important for antiviral skin reactions. Keratinocytes are active antiviral protection of the skin since they increase the production of interferons I, II, and III during infection, suppressing the reproduction of the virus. The skin response of interferon to viral infections looks like superficial dermatitis.
Interferon is Involved in Autoimmune Skin Diseases
Interferonopathy
In type I interferonopathies, the transmission of interferon signals is enhanced as mutations occur in the genes responsible for the perception of nucleic acids. These mutations lead to a steady increase in interferon levels.
Patients with Aicardi-Gutierrez syndrome usually have encephalopathy and a skin lesion similar to cutaneous lupus erythematosus. Mutations in genes lead to the accumulation of nucleic acids and enhanced production of IFN-I. An increase in the production of IFN subsequently leads to hyperactivation of immunity.
Patients with mutations of the TMEM173 gene, which encodes the STING – stimulator protein of interferon genes, have lupus-like zygomatic rash and alopecia in the background of systemic pulmonary fibrosis and arthritis. This disease is called STING-associated vasculopathy with onset in infancy (SAVI).
Numerous studies show that mutations of the SAMHD1 gene, which regulate the innate immune response, are associated with mouth ulcers, joint pain, and skin lesions similar to frostbite.
All these are hereditary disorders in the transmission of interferon signals, which cause lupus-like skin lesions and indicate the critical role of IFN in skin inflammation.
Cutaneous Lupus Erythematosus
Cutaneous lupus erythematosus (CLE) includes several skin inflammations associated with systemic lupus erythematosus (SLE) but may also be an independent disease.
CLE is present in most patients with SLE and is often triggered or aggravated by ultraviolet light. The pathogenesis of CLE is not completely clear, but it is believed that elevated interferon levels, especially IFN-I, play a central role in the development of CLE lesions. IFN-I response in peripheral blood and skin correlates with disease activity.
In CLE, interferon-stimulated genes are strongly expressed in the epidermis and dermis. Of the studied interferons, the levels of IFN-alpha-10 and IFN-kappa are the most elevated in the skin with CLE.
In CLE, IFN-I is produced in response to skin triggers, such as ultraviolet radiation. Photosensitive lesions are characterized by increased cell death, inflammatory cell infiltrates, and the involvement of plasmacytoid dendritic cells. These cells are attracted by chemokines and other proteins, the level of which increases when stimulated by interferon. UV radiation also stimulates the attraction of pDC. pDC produces IL-21 protein that activates cytotoxic T cells that destroy keratinocytes.
UV radiation enhances the skin response of interferon and increases IFN-induced inflammation in CLE compared to healthy skin. A broad-spectrum sunscreen protected the skin from inflammation in CLE.
UV radiation stimulates the immune response to the body’s nucleic acids, increasing the production of IFN in keratinocytes. Sustained overexpression of IFN-kappa contributes to the death of keratinocytes caused by UV radiation. Blockade of interferon signaling with baricitinib suppresses the death of keratinocytes caused by UV-B radiation in SLE.
Interferons of types II and III are also involved in the pathogenesis of CLE. In the peripheral blood of patients with CLE, the level of IFN-gamma is elevated, while IFN-gamma suppresses the growth of keratinocytes. In addition, IFN-gamma increases with CLE and is produced by keratinocytes in response to stimulation of poly-IC, which is used to simulate a viral infection.
A clinical study showed that IFN-gamma blockade reduces the expression of the IFN-gamma gene in CLE lesions and reduces the proinflammatory cytokine CXCL10 in serum.
Dermatomyositis
Dermatomyositis (DM) is a chronic autoimmune disease accompanied by diffuse inflammation of connective tissue and affects muscles, skin, and organs such as the lungs and heart. Skin symptoms of DM significantly reduce the quality of life of patients. Skin manifestations include a blue-purple heliotrope rash on the upper eyelids combined with edema, a flat red rash on the face and upper torso, and erythema of the finger joints that do not affect the phalanges of the fingers and is accompanied by purple scaly rashes.
In patients with dermatomyositis, the level of interferon-stimulated type I genes (ISG) is increased. A high level of ISG in peripheral blood correlates with the activity of the disease. In the skin with DM, the level of ISG also increases.
Sjogren’s Syndrome
Sjogren’s syndrome (SS) is an autoimmune disease in which the exocrine glands become inflamed and which leads to dry eyes (dry keratoconjunctivitis) and dry mouth (xerostomia). SS is often combined with systemic lupus erythematosus. Skin manifestations occur in 16-50% of patients with SS and may include: dry skin, inflammation of the corners of the mouth with the formation of cracks, dermatitis of the eyelids, itching, ring-shaped erythema, and inflammation of the walls of blood vessels.
ISG expression is increased in the peripheral blood of patients with SS. It is important to note that recent reports of clinical cases show that hydroxychloroquine, which reduces the production of type I IFN, may be an effective treatment for cutaneous SH.
Psoriasis
Psoriasis is a chronic autoimmune disease that affects the skin and can affect nails and joints. Clinically, skin lesions are characterized by erythema, excessive epidermis growth, and peeling.
Psoriasis is associated with a violation of the regulation of the immune response in the skin. In psoriasis, T cells are activated, which migrate into the skin and secrete the inflammatory cytokine TNFa. TNFa increases the proliferation of keratinocytes, which leads to excessive growth of the epidermis.
In multiple sclerosis or hepatitis C, interferon treatment aggravates existing psoriatic plaques or causes new lesions that disappear when therapy is discontinued. In addition, medications such as imiquimod, which lead to an increase in the production of IFN, cause psoriatic skin disease.
However, systemic antimalarial drugs, such as hydroxychloroquine, which suppress the transmission of interferon signals, are also associated with an exacerbation of psoriasis. The reason may be a violation of the regulation of TNFa, a key cytokine in the pathogenesis of psoriasis.
Drugs that suppress TNFa are used to treat psoriasis. However, 2-5% of patients treated develop psoriasis-like lesions called paradoxical psoriasis. Interestingly, the skin in paradoxical psoriasis is characterized by overexpression of type I IFN and accumulation of pDC and does not depend on T cells compared to classical psoriasis.
The interferon-stimulated DDX58 gene is an essential factor of susceptibility to psoriasis. DDX58 participates in antiviral reactions and encodes the innate antiviral RNA receptor RIG-I, which regulates the production of interferons of types I and II. The level of RIG-I increases in the skin with psoriasis and is activated by double-stranded RNA, which causes the production of the inflammatory cytokine IL-23 and triggers psoriasis-like skin disease in mice. IL-23 is a crucial cytokine in psoriasis, as it promotes the survival and proliferation of T-helper cells that stimulate the reproduction of keratinocytes. Blocking IL-23 leads to clinical improvement of psoriasis.
In addition, IFN-I enhances the expression of the IL-22 protein receptor on keratinocytes and stimulates the proliferation of keratinocytes and the growth of the epidermis.
IFN-alpha and IFN-beta are activated in the skin with psoriatic lesions. Increased expression of IFN-alpha/beta in mice leads to the development of psoriasis-like skin disease. Imiquimod, which activates pDC and stimulates the production of type I interferon, also causes psoriasis in mice. At the same time, if, after binding IFN to the interferon receptor, IFN signaling is not suppressed, skin inflammation caused by imiquimod is aggravated.
IFN-alpha is temporarily produced in the early stages of psoriasis development, and the type I IFN signaling pathway is activated in psoriatic keratinocytes. Unlike normal skin, psoriatic plaques have elevated levels of IFN-I and associated ISG. A clinical study of a monoclonal antibody against IFN-alpha failed to show clinical benefit in patients with chronic psoriatic plaques, confirming the hypothesis that IFN is involved in the initiation of psoriasis but not in the formation of chronic plaques.
Lichen Planus
Lichen planus (LP) is a chronic inflammatory disease of the skin, mucous membranes, and nails. LP lesions are itchy purple polygonal papules or plaques. LP is an autoimmune disease in which autoreactive T–killers damage basal keratinocytes.
As in the case of psoriasis, interferon-alpha treatment triggers or exacerbates lichen planus. Lichen planus is associated with chronic hepatitis C infection, which confirms the role of antiviral signals in the occurrence of skin inflammation. In patients with LP, interferon-stimulated genes are higher than in healthy people. At the same time, the level of ISG in LP is higher in patients with hepatitis C than in patients without hepatitis C.
Interferon-gamma also triggers cytotoxic inflammation in LP. In peripheral blood and lesions of the skin and mucous membranes with LP, the expression of IFN-gamma-stimulated genes increases.
Localized scleroderma (morphea)
Localized scleroderma is an inflammatory sclerosing disease that affects the skin and subcutaneous tissue.
It is believed that vascular damage is the initial stage of sclerosis. Vascular damage contributes to the attraction of inflammatory cells and the production of profibrotic cytokines, leading to collagen destruction. Interferon-producing plasmacytoid dendritic cells are abundant around the vessels and fibrous bundles of the affected localized skin scleroderma.
Treatment with IFN-beta can cause localized scleroderma. In addition, localized scleroderma coincides with other diseases in the pathology in which IFN-I is involved. Among them are lupus, Sjogren’s syndrome, and alopecia areata. In foci of fibrosis with localized scleroderma, the level of MXA protein increases, which is regulated by type I interferon.
Alopecia areata
Alopecia areata (AA) is a disease in which the immune system attacks the hair follicles, leading to hair loss in certain areas or the entire body.
Treatment with type I interferon may contribute to the occurrence of AA. Elevated levels of IFN-gamma in the skin affected by alopecia contribute to the production of chemokines CXCL9 and CXCL10, which enhance the reaction of T cells to hair follicles, which leads to hair follicles damage and hair loss.
A clinical study has shown that suppression of interferon signaling is effective for treating alopecia areata, although it brings only temporary results.
Vitiligo
Vitiligo is a depigmenting autoimmune disease caused by the destruction of epidermal melanocytes. Vitiligo lesions are challenging to treat, and the only approved therapy is monobenzone cream, which depigments normal skin.
The expression of IFN-gamma and chemokines CXCL9 and CXCL10, whose production is stimulated by IFN-gamma, is increased in the skin and serum of patients with vitiligo. These chemokines attract T-killers into the skin, contributing to the destruction of melanocytes. CXCL10 is necessary for the progression of vitiligo and the maintenance of depigmentation. Neutralization of CXCL10 returns pigmentation to the skin.
Conclusions
Type I interferon is responsible for the antiviral response and skin protection from infections. Skin cells keratinocytes produce IFN-kappa. A balance of IFN signaling is necessary to maintain optimal skin health. Chronic increase in IFN production contributes to skin inflammation in various diseases.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
The Influence of Interferon on Healthy and Diseased Skin