Content
- What factors predispose fungal diseases
- Candidiasis Associated with Coronavirus Deaths
- COVID-19 complication: Facial palsy associated with a fungal infection
- Mycosis and interferon system
- How interferon works in fungal infections
- Interferon-Gamma Role in Mucocutaneous and Invasive Candidiasis
- Type I, II and III interferons in aspergillosis
- Interferon-Gamma in Cryptococcosis
- Interferon-gamma to treat fungal infections
- Type I Interferon Protects against Intestinal Candidiasis
- Interferon-alpha-2b to treat thrush
- Type I interferon enhances tissue damage in fungal sepsis
- Vitamin D3 Destroys Candida and Reduces the Risk of Systemic Thrush
- Interferon α2b and Vitamin D Reduce Candida-induced Inflammation of the Vaginal Mucosa in Pregnancy
- Conclusion
- References
What Factors Predispose Fungal Diseases
Fungi accompany a person throughout life. They can live on the skin, mucous membranes, and in intestines. Fungal spores enter us through breathing, eating, or skin injuries.
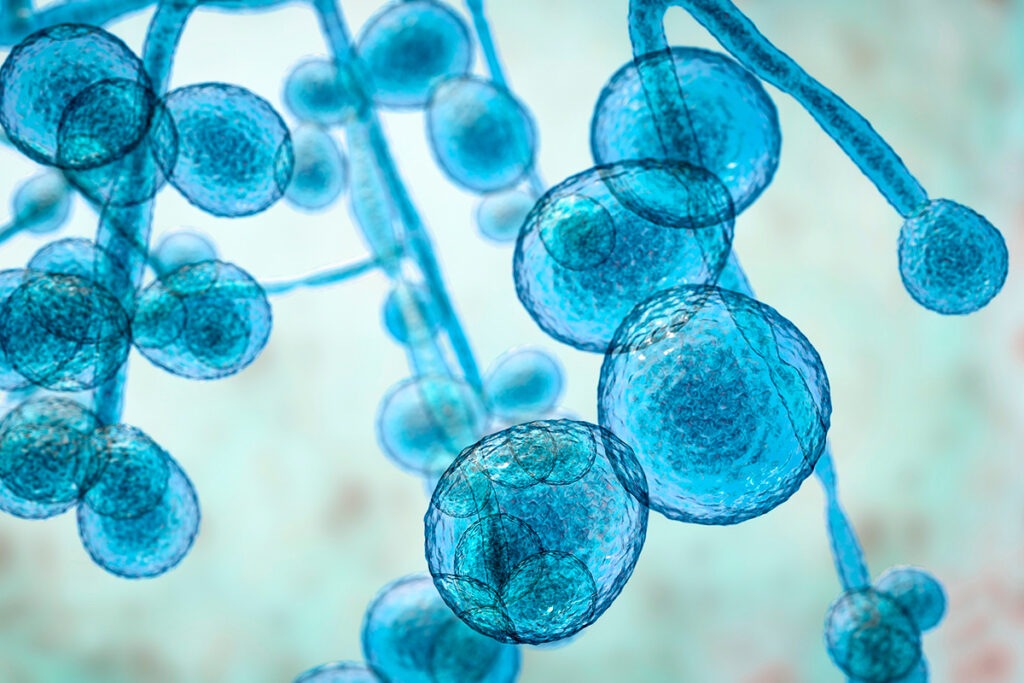
Of the 5 million known species of fungi, about 100 species are capable of causing human disease.
Mycosis is an infectious disease in humans and animals caused by a pathogenic fungus. In 2010, fungal infections were the fourth most common skin disease. Mycoses affect the skin, mucous membranes, nails, and hair. Fungal infections can also affect the lungs, other internal organs, and the brain.
The frequency of fungal infections is currently increasing due to several reasons:
- Use of broad-spectrum antibiotics. Antibiotics can disturb the microflora, which allows fungi to multiply uncontrollably
- Metal and plastic dentures are a favorable environment for fungi
- Invasive monitoring and procedures that open the way for fungal infections
- Parenteral nutrition (through a vein) provides nutrients and fungi
- Suppressed immunity in autoimmune and rheumatological diseases
- Cancer chemotherapy
- Transplantation of internal organs
- AIDS
- Drug addiction
- Tourism to countries with a hot climate where endemic mycoses occur
In addition, new risk groups have emerged for patients with severe fungal diseases associated with respiratory viruses and patients receiving monoclonal antibodies or Janus kinase inhibitors for autoimmune, inflammatory, or neoplastic diseases. Human health is also threatened by a new species of fungus – Candida auris, which has drug resistance. Fungi can cause superficial and life-threatening invasive infections, especially in immunocompromised people.
Mortality from severe fungal infections affecting the body’s organs and systems is 85-90%.
Often the treatment of fungal infections is ineffective because fungal infections do not have specific signs and symptoms, diagnostic tests are unreliable enough, and antifungal drugs are weak or not broad enough. Therefore, new methods are needed for the treatment of fungal diseases.
Antifungal activity of immune cells stimulates by acting on the interferon system to enhance the effectiveness of the treatment of mycoses.
Candidiasis Associated with Coronavirus Deaths
Coronavirus increases susceptibility to fungal infection. Excessive production of pro-inflammatory cytokines in COVID-19 may lead to hyperactivation of the immune system, promoting tissue damage and fungal invasion. Also, candidiasis is facilitated by a decrease in the level of lymphocytes, which is observed in patients with COVID-19. The likelihood of candidiasis increases the use of corticosteroids and antimicrobials, and intravenous catheters.
Greek scientists examined body tissue samples from 1,536 elderly patients hospitalized with coronavirus. Candida fungus was found in 4.5% of patients. Most often, Candida was found in urine samples and was not associated with invasive candidiasis. However, invasive candidiasis was confirmed in 0.8% of patients – the Candida fungus was found in the blood and bronchi.
Invasive candidiasis worsens the course of coronavirus and increases mortality. Compared to other COVID-19 patients, Candida-positive patients were older, had more extended hospital stays (22 days), and had higher overall mortality (34.8%). Testing for Candida may be necessary for determining the mortality risk in patients with COVID-19.
Details of the study are in the article “Fungal Infections with Coronavirus.” The study is published in the Diagnostics journal.
COVID-19 complication: Facial palsy associated with a fungal infection
Fungal infections are one of the complications of COVID-19. Mucormycosis is a fungal infection that develops in conditions of suppressed immunity. Coronavirus is associated with a state of immunosuppression, a factor predisposing to fungal infection.
The most common form of mucormycosis is rhino cerebral (30-50% of cases). Symptoms include unilateral headache behind the eye, swelling of the eye area, and facial paralysis.
60-80% of cases of mucormycosis occur in patients with diabetes mellitus. Diabetes mellitus is associated with immunodeficiency. Hyperglycemia stimulates the fungus’s reproduction and reduces phagocytic activity, allowing the fungus to grow. In patients with uncontrolled diabetes and mucormycosis, facial paralysis occurs in 11% of cases.
Also, facial paralysis is one of the complications of coronavirus. American scientists described the cases of three diabetic patients who developed facial paralysis after the coronavirus and were diagnosed with mucormycosis. Rhino cerebral mucormycosis affects the pterygopalatine fossa and could spread to the facial nerve. Mucormycosis, hyperglycemia, and the recent coronavirus were associated with facial paralysis in all three patients.
Expansion of the pterygopalatine fossa, seen on MRI, can be used to detect damage to the facial nerve.
Details of the study can be found in the article “COVID-19 Complication: Facial Nerve Palsy Associated with Fungal Infection.” The study was published in The Cureus Journal of Medical Science.
Mycoses and the interferon system
Interferons (IFN, IFN) are molecules that trigger an immune response against infectious agents.
The predisposition to fungal infection depends on the functioning of the interferon system. In 2013, a group of scientists from leading universities in the US and the Netherlands compared the genes of healthy volunteers and people predisposed to chronic fungal infection. The researchers studied the function of immune blood cells when exposed to the fungus Candida. The most active were the genes associated with the IFN system. Some of these genes have been disrupted due to mutations in people prone to chronic fungal infection. Some mutations disrupted the production of IFN, and other mutations reduced the biological activity of interferon molecules.
A Delicate Balance Of Type I Interferon Protects Against Fungal Infections
After entering the body, fungi activate the fungal pathogen recognition receptor Dectin-1 on the surface of dendritic cells, briefly stimulating the production of a small amount of IFN-beta. When started by Dectin-1, dendritic cells alter the function of T helper cells (Th cells) to generate an immune response.
Under the influence of a small amount of IFN-beta, T-helpers develop into non-pathogenic Th17 cells in normal conditions. These cells produce the pro-inflammatory cytokine IL-17 and the anti-inflammatory cytokine IL-10, helping to suppress fungal infection without causing tissue damage.
However, if too much type I interferon or the functioning of the interferon receptor is disrupted, then an increased number of pathogenic Th17 cells develop. These cells produce the pro-inflammatory cytokines IL-17 and IFN-gamma, causing inflammation and tissue damage.
Pathogenic Th17 cells develop because when the interferon response is impaired, dendritic cells stop producing the cytokine TGFβ, which is necessary for developing non-pathogenic Th17 cells. TGFβ blocks the production of the pro-inflammatory cytokine IFN-gamma in T cells.
Thus, errors in Dectin-1 signaling and/or impaired type I interferon response can develop severe fungal infections. Restoration of a normal IFN-I response may attenuate the pathogenesis of the disease.
Details of the study on the response of interferon in fungal infections can be found in the article “A Delicate Balance of Type I Interferon Defeats Fungus”. The study is published in the journal Nature Immunology.
How Does Interferon Work in Fungal Infections
Interferon activates immune phagocyte cells’ antifungal response that destroys fungal cells and spores. Fungal cells are protected from external influences with the help of chitin and melanin, which are part of their cell membrane. Therefore, phagocytes produce reactive oxygen species (ROS) to destroy the membrane of the fungus and damage its DNA. Interferons stimulate phagocytes to produce large amounts of ROS. Violations in the work of this mechanism lead to chronic fungal diseases, damage to internal organs, and sepsis.
In 2017, American scientists showed that type III IFN is necessary for the antifungal response of neutrophils, cells of innate immunity that destroy fungi and other pathogens. Mice with a genetic defect in the IFN-III response died from a fungal infection. However, the introduction of type I IFN stimulated the expression of IFN-III, restored the production of reactive oxygen species in phagocytes, and improved survival.
Young animals and humans are more susceptible to invasive fungal infections because of the reduced activity of neutrophils, which destroy the pathogens of fungal infections worse, as well as the fact that the spleen cells of young animals produce less IFN-gamma (type II interferon). The introduction of IFN-gamma can restore the activity of neutrophils to the level of adults and increase the survival of young animals.
However, type I interferon in invasive fungal infections can play a detrimental role:
- During infection with Candida parapsilosis, IFN-I triggered the production of IL-27, which worsened the clearance of the fungus.
- 7 days after infection with Candida glabrata, IFN-I promoted chronic fungal infection, although there was no such effect in the later stages of the disease.
In systemic fungal infections, type I interferons worsen the course of the disease, interfering with antifungal defense processes:
- IFN-β triggered the expression of ISG IFIT2, and IFIT2 suppressed the production of reactive oxygen species, which cells use to kill the fungus. In mice, IFN-β contributed to pathology and death from candidiasis.
- In Candida glabrata infection, IFN-I caused iron to accumulate in macrophages, the cells that engulf and digest the fungus. After macrophages took over Candida glabrata, the fungus gained access to iron, which promoted the reproduction of the fungus inside the cells and protected it from the immune response.
Type I interferon is essential for antifungal immunity. Italian scientists have found that Candida spp. and Saccharomyces cerevisiae induce a protective interferon-beta response in the body. In addition, after intravenous administration of Candida albicans to mice, most of the mice lacking the IFN-alpha/beta receptor died from uncontrolled fungal growth. However, mice with a regular interferon system survived.
IFN-I-related genes are essential for human antifungal defense. Mutations in genes associated with IFN-I increase the likelihood of the fungus entering the bloodstream:
- MDA5 is one of the receptors that trigger the IFN-I response. Mutations in the IFIH1 gene, which encodes the MDA5 receptor, increase susceptibility to candidiasis and aspergillosis.
- IFN-I is involved in protection against aspergillosis, which is secreted after activation of pattern recognition receptors TLR3 and Dectin-1. IFN-I is produced during lung infection by Aspergillus fumigatus and stimulates the antifungal activity of neutrophils through IFN-III signaling.
The article “Type I Interferons in Fungal Infections” reviews the response of IFN-I to Candida and Aspergillus fumigatus infections. The study was published in the PLOS Pathogens journal.
Interferon-Gamma Role in Mucocutaneous and Invasive Candidiasis
The yeast Candida (primarily Candida albicans) lives in most people’s gastrointestinal and reproductive tracts without causing harm. When the immune system or the balance of the microbiota is disturbed, Candida turns into a pathogen and can cause mucocutaneous fungal infections, enter the bloodstream and cause invasive candidiasis, infecting deep-seated organs – the liver, spleen, and kidneys.
Congenital and adaptive lymphocytes are required to protect against mucocutaneous candidiasis, and myeloid phagocytes are necessary to protect against invasive candidiasis. Thus, HIV/AIDS patients with a low level of T-helpers have an increased risk of developing mucocutaneous candidiasis, while patients with a reduced level of neutrophils (phagocytes) are prone to invasive candidiasis, but not vice versa.
Mucocutaneous Candidiasis
Mucocutaneous candidiasis presents clinically as oropharyngeal candidiasis (OPC), esophageal candidiasis, or vulvovaginal candidiasis (VVC).
To protect against mucocutaneous candidiasis, the pro-inflammatory cytokine IL-17, produced by TH17 cells, is required. Mucocutaneous candidiasis is associated with decreased levels of circulating TH17 cells and an excessive interferon-gamma (IFN-gamma) response.
In autoimmune diseases, mucocutaneous candidiasis is promoted by mucosal immunopathology with an attenuated or excessive IL-17 response and neutralizing antibodies to IL-17, which are associated with chronic mucocutaneous candidiasis (CMC).
Excess production of IFN-gamma by mucosal T cells can increase susceptibility to OPC, causing inflammation and disruption of the epithelial barrier. Suppression of IFN-gamma signals improves symptoms.
Invasive Candidiasis
The use of antibiotics is associated with the development of invasive candidiasis. Broad-spectrum antibiotics cause intestinal dysbiosis, impair the intestinal immune response, reduce intestinal TH17 levels, and suppress local production of antimicrobial peptides, increasing colonization of the intestine by Candida and facilitating the penetration of the fungus into the internal organs.
Immunosuppression, chemotherapy-induced neutropenia, or corticosteroids impairs the antifungal response of myeloid phagocytes and promotes Candida invasion.
Although neutrophils are protective during invasive candidiasis, their excessive accumulation and activation can also have deleterious effects, seen in neutropenic patients after neutrophil recovery. IFN-gamma promotes the activation of neutrophils and their migration to the site of infection. Neutrophils release cytokines that increase inflammation. In this situation, corticosteroids relieve inflammation and clinical symptoms.
The study was published in the Nature Reviews Immunology journal.
Type I, II and III interferons in aspergillosis
Aspergillosis is an immune-suppressed, life-threatening fungal infection that develops after inhalation of the ubiquitous Aspergillus molds, primarily Aspergillus fumigatus.
Aspergillosis can develop in people with reduced levels or dysfunction of myeloid phagocytes, such as neutropenia, patients receiving corticosteroids or stem cell transplants, and patients with severe influenza or COVID-19 pneumonia.
Myeloid phagocytes are essential for protection against aspergillosis. Aspergillosis is a common infection in chronic granulomatous disease associated with phagocyte dysfunction. In chronic granulomatous disease, phagocytes produce poorly reactive oxygen species (ROS), which are needed to suppress bacteria and fungi.
IFN-gamma stimulates the production of ROS by phagocytes. Therefore, recombinant IFN-gamma has been approved for immunotherapy to prevent invasive, including fungal, infections in patients with chronic granulomatous disease.
Type I and III interferon signaling is essential for antifungal protection, as it enhances ROS production by neutrophils, stimulating the destruction of fungi. Janus kinase is required for IFN signaling. Janus kinase inhibitors contribute to the development of aspergillosis.
The study was published in the Nature Reviews Immunology journal.
Interferon-Gamma in Cryptococcosis
Cryptococcosis is caused by the yeast fungi Cryptococcus neoformans and Cryptococcus gattii:
- neoformans is more common and usually causes meningoencephalitis in immunocompromised patients with T-helper depletion or dysfunction. Often, cryptococcal meningoencephalitis affects AIDS patients and remains a common cause of death in areas where antiretroviral therapy and antifungals are not available. However, the incidence of cryptococcal meningoencephalitis is also increasing among people who are not infected with HIV.
- In contrast, C. gattii usually causes lung disease in immunocompetent people and rarely affects people with HIV/AIDS.
Cryptococcus is often present in the droppings of pigeons and other wild birds. Cryptococcosis develops by inhalation of dust from soil contaminated with fungi.
Resident pulmonary macrophages protect against the reproduction of the fungus in the lungs and infection of other body tissues. IFN-gamma, produced by T-helpers, provides the activation of macrophages and the destruction of the fungus.
Disruption of IFN-gamma production by T cells results in the inability of macrophages to destroy the fungus. Also, cryptococcosis develops in patients with neutralizing autoantibodies to IFN-gamma. Possible treatments for these patients are drugs that deplete B cells and antibody-secreting plasma cells.
The following medications increase the risk of cryptococcosis:
- Janus kinase inhibitors block IFN-gamma receptor signaling.
- TNF inhibitors disrupt the production of IFN-gamma and the formation of foci of inflammation.
- Bruton’s tyrosine kinase inhibitors disrupt the activation of macrophages.
Interruption of IFN-gamma signaling in macrophages impairs nitric oxide production, which is necessary for destroying fungi, allowing Cryptococcus to survive after ingestion by the phagocyte. In HIV/AIDS patients, the lack of T-helpers, macrophages, and pro-inflammatory cytokines IFN-gamma and TNF in the cerebrospinal fluid is associated with severe cryptococcosis in the central nervous system (CNS). A T cell response with IFN-gamma and TNF is associated with increased survival.
IFN-gamma increases the antifungal activity of macrophages in patients with HIV/AIDS without T-helpers. IFN-gamma immunotherapy rapidly reduces the fungal burden in the cerebrospinal fluid, improving patient survival.
Although T helpers are critical in fighting fungi, these cells can also worsen cryptococcosis in patients without HIV or in patients with immune reconstitution inflammatory syndrome (IRIS) in HIV. IRIS is a life-threatening complication after starting antiretroviral therapy.
In patients without HIV with cryptococcosis, there is a significant infiltration into the CNS of T-helper cells with the CXCR3 receptor on the surface. One of the proteins that the CXCR3 receptor binds to is CXCL10, produced in response to IFN-gamma. When the CXCR3 receptor binds to the CXCL10 protein, T-helpers and macrophages are attracted to the site of infection. CNS infiltration of T-helper cells in non-HIV patients with cryptococcosis has been associated with high levels of the CXCL10 protein in the cerebrospinal fluid. Although the attraction of tissue macrophages to the site of infection was not impaired, these macrophages acquired anti-inflammatory properties, and fungal phagocytosis was impaired. As a result, non-HIV patients with cryptococcosis developed neuronal damage. In a study in mice with non-HIV-associated cryptococcosis, downregulation of CXCR3 countered the recruitment of T helpers to the CNS and increased survival.
AIDS patients with IRIS have increased T-helper type 1 and elevated serum IFN-gamma compared to patients without IRIS. In a mouse model of cryptococcosis in IRIS, IFN-gamma-producing T helpers were sufficient to cause cerebral edema and CNS damage.
The study was published in the Nature Reviews Immunology journal.
Interferon-Gamma to Treat Fungal Infections
Interferon-gamma promotes the development of specialized phagocytes that most effectively suppress fungal infection. In 2014, scientists at the Radboud University Medical Center (Netherlands) investigated the effectiveness of interferon-gamma as part of complex antifungal therapy. All patients had a severe fungal infection affecting the internal organs, and the immune system was suppressed. Interferon-gamma contributed to the partial restoration of immune function. In patients, a week after the start of treatment, the number of specialized phagocytes, which play an essential role in antifungal protection, doubled.
Interferon-gamma is effective against intracellular and extracellular fungi, dimorphic fungi of endemic mycoses, and opportunistic fungal microorganisms. Scientists at Stanford University have shown that IFN-gamma enhances the antifungal activity of immune effector cells, monocyte-macrophage cells, and neutrophils. Interferon-gamma activated tissue macrophages that destroyed fungal pathogens such as Blastomyces dermatitidis, Paracoccidioides brasiliensis, Candida albicans, and pulmonary macrophages destroyed Blastomyces, Paracoccidioides, and Histoplasma. In addition, IFN-gamma activates neutrophils, increasing the release of reactive oxygen species that kill the fungus.
Scientists have investigated the effectiveness of interferon-gamma in the treatment of fungal infections. Studies were conducted both on animals and on patients with mycoses:
- In chronic paracoccidioidomycosis, the introduction of IFN-gamma enhanced the effect of antifungal therapy.
- IFN-gamma is essential for the immune response in the brain in cryptococcosis. Cryptococcosis was severed in mice with impaired IFN-gamma response. The administration of interferon-gamma with antifungal therapy improved the survival of mice and increased the antifungal drug amphotericin B 40-fold.
- In a pilot placebo-controlled study, IFN-gamma was administered as an adjunct to traditional chemotherapy for cryptococcosis in HIV-positive people. The combination of antifungal drugs with interferon-gamma accelerated the sterilization of cerebrospinal fluid and reduced the clinical manifestations of mycosis.
- IFN-gamma reduced the risk of systemic candidiasis.
For more information on the mechanisms of action of IFN-gamma, see the article “Interferon-gamma for the treatment of fungal infections.”
Type I Interferon Protects against Intestinal Candidiasis
Epithelial cells are responsible for forming innate immunity on the surfaces of the mucous membrane. They provide tolerance in case of harmless microbes or trigger a defensive reaction in case of infection.
IFN-I regulates epithelial responses and can be both pro- and anti-inflammatory. Intestinal cells respond to IFN-I signaling, allowing the immune system to distinguish between harmless microorganisms and pathogens.
Probiotics increase the production of IFN-α in the intestine, curbing inflammation and shaping the composition of the intestinal microbiota, thereby inhibiting the growth of Candida.
Interferon-Alpha-2b to Treat Thrush
Thrush is a disease caused by opportunistic fungi Candida albicans (C. albicans). Usually, C. albicans is present in the vagina in small amounts and does not cause disease. However, when immunity is reduced, or the microflora is disturbed, C. albicans multiply excessively, causing symptoms of thrush:
- itching, soreness, and irritation of the vulva;
- pain or discomfort during sex or urination;
- vaginal discharge, often white curdled;
- vulvovaginal inflammation, redness of the vagina and vulva.
Thrush affects 75% of women of reproductive age. Thrush is also called vulvovaginal candidiasis. Candida albicans cause 85-90% of cases of vulvovaginal candidiasis.
At an early stage of Candida infection, the vaginal mucosa reacts by transmitting IFN-I signals and stimulating ISG expression. At this stage, the epithelium is not yet damaged, and the fungus does not cause harm. With excessive Candida reproduction, IFN-I no longer increases, and fungi violate the mucous barrier, leading to cell damage.
In thrush, different types of IFN-I are produced in different ways:
- Healthy women have higher levels of IFN-β in the vaginal fluid than those with vulvovaginal candidiasis.
- However, the level of IFN-α is increased in patients with vulvovaginal candidiasis.
Three main types of drugs are used to treat thrush: polyenes, azoles, and echinocandins. However, some strains of C. albicans are resistant to antifungal drugs. This problem poses a vital task for scientists – to find new methods of treatment and prevention of fungal diseases.
Chinese scientists have shown that interferon-alpha-2b is necessary for antifungal immunity, inhibits the reproduction and growth of C. albicans fungi, and accelerates the recovery of vaginal epithelial cells:
- IFN-alpha-2b enhances local vaginal cellular immunity before infection, stimulating a rapid response to C. albicans and providing enhanced protection for the vaginal epithelium.
- IFN-alpha-2b promotes the T-helper response 17. These cells support mucous membranes and protect against fungal and bacterial infections.
- IFN-alpha-2b stimulates the secretion of non-B-cell IgG antibodies. The classical concept of antibody production suggests that only B cells secrete IgG. However, healthy vaginal epithelial cells can also secrete functional IgG antibodies. This form of IgG is involved in the innate vaginal immune response against fungal infections, similar to traditional IgG expressed by B cells.
In another study, Chinese scientists evaluated the effectiveness of recombinant interferon-alpha-2b for thrush treatment. The study was carried out on rats. Interferon-alpha-2b inhibited the growth of Candida albicans by 50% in thrush, reduced inflammation, reduced the degree of damage to the tissues of the vagina, restored the thickness of the epithelium, and also enhanced the immune response against candidiasis.
Type I interferon is required to activate antifungal immunity in vaginal epithelial cells. IFN-alpha-2b can be used to treat vulvovaginal candidiasis in parallel with antifungals to improve patient outcomes.
Details of the study are located in the article “Interferon-Alpha-2b Improves The Effect of Antifungal Drugs in Thrush Treatment.”
Type I Interferon Enhances Tissue Damage in Fungal Sepsis
Fungal sepsis is a systemic inflammation that occurs in response to the penetration of the fungus into the blood. Sepsis in invasive candidiasis can lead to the inadequate blood supply to tissues and organs and multiple organ failure syndromes, including acute renal failure. Candida is one of the most common pathogens found in fungal sepsis.
Although the type I interferon response plays a protective role in the early stages of fungal infection, in later stages, IFN-I can cause tissue damage. In the early stages, interferon prevents the development of severe candidal conditions by stimulating the inflammatory action of phagocytic cells – monocytes and neutrophils. However, interferons’ uncontrolled activation of these cells during sepsis can increase systemic inflammation and contribute to fatal tissue damage.
Progressive sepsis combined with renal failure is a common cause of death in severe fungal infections. The degree of damage to the kidney tissue is related to the level of the innate immune response. Therefore, in sepsis, it is not so much the Candida fungus that worsens the outcome of the disease but the uncontrolled inflammatory response.
In a mouse study, blocking the type I interferon receptor reduced the activity of inflammatory myeloid cells and rendered mice resistant to deadly candidal infections. In the same survey, pharmacological suppression of inflammatory monocytes and neutrophils with the antidiabetic drug pioglitazone reduced renal immunopathology and improved survival in mice.
Vitamin D3 Destroys Candida and Reduces the Risk of Systemic Thrush
Candidemia is an infection of the blood by the fungus Candida, the most common systemic fungal infection. The prevalence of candidaemia in pediatric intensive care units (ICUs) has increased dramatically over the past decade. Candidemia often leads to severe illness and increases mortality among hospitalized patients.
Amphotericin B is commonly used to treat systemic fungal infections. Nevertheless, amphotericin B can cause severe side effects, affecting not only fungal membranes but also the membranes of body cells and destroying them. In addition, in the last few years in clinical practice, there have been cases of candidiasis resistant to antifungal treatment. Therefore, finding new drugs to treat mycoses is crucial, which can suppress and destroy the fungus’s growth.
Taking vitamin D during antibiotic therapy will help prevent Candida infection:
- A laboratory study by Algerian scientists showed that 100mg/ml of vitamin D3 significantly inhibited the growth of Candida albicans. The antifungal effect may be since vitamin D3 is fat-soluble and, therefore, can alter the integrity of the cell membrane, the main component of which is fat.
- A clinical study by Chinese scientists showed that yogurt supplemented with vitamin D3 reduced the incidence of candidemia and candiduria and the length of ICU stay. The study participants were children who received a broad-spectrum antibiotic and were in the ICU.
Details of the studies are in the article “Vitamin D3 – a new remedy against fungal infections.” Sources are ScienceDirect and The Journal of Human Nutrition and Dietetics.
Interferon α2b and Vitamin D Reduce Candida-induced Inflammation of the Vaginal Mucosa in Pregnancy
Pregnant women are often deficient in vitamin D, with more than 50% of cases of vaginal infections. Vitamin D deficiency can increase inflammatory responses, causing more severe conditions and risks to the fetus. In treating infectious diseases in pregnant women, restoring the balance of pro-inflammatory and anti-inflammatory cytokines is vital. In clinical practice, interferon α-2b preparations are used for this.
Russian scientists studied how vitamin D and interferon α-2b affect the level of inflammation and antiviral protection as part of the complex treatment of vaginal infections in pregnant women. Most often, pregnant women have experienced inflammation of the vaginal mucosa caused by the fungus Candida albicans. Pregnant women received antibiotic therapy.
In addition to antibiotic therapy, vitamin D and interferon alfa-2b reduced inflammation by lowering the pro-inflammatory cytokine IL-8 levels in healthy pregnant women. Vitamin D increased interferon-gamma levels and enhanced antimicrobial protection – pregnant women who took vitamin D were 11 times less likely to suffer from acute respiratory infections.
Details of the study can be found in the article “Interferon α2b and Vitamin D Reduce Inflammation in Vaginal Infections in Pregnancy.” The study was published in the journal Infection and Immunity.
Conclusion
Interferons can have both positive and detrimental effects on fungal diseases:
- Treatment of IFN-I may be helpful for candidiasis of the mucous membranes but not for systemic.
- In vulvovaginal candidiasis, IFN-α increases the resistance of the epithelium to infection and reduces inflammation.
- In aspergillosis, IFN-I improves antifungal immunity and the outcome of the disease.
- IFN-I is essential for maintaining the intestinal barrier and can reduce the penetration of Candida albicans through the intestinal barrier.
- In fungal sepsis, type I interferon increases systemic inflammation and promotes tissue damage. Pharmacological suppression of inflammatory monocytes and neutrophils may improve the outcome of invasive candidal infections.
At the same time, interferon is essential for antifungal immunity. In the early stages of mycoses, interferon prevents disease progression.
Interferon preparations stimulate a person’s interferon system. Interferon is universal in its action and can suppress both known and new types of fungi. Interferon enhances the effectiveness of standard antifungal therapy.
An important field of application of interferons is the prevention of fungal diseases in people with immune genetic abnormalities and reduced immunity.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
- Immune responses to human fungal pathogens and therapeutic prospects
- Candida Species Isolation from Hospitalized Patients with COVID-19—A Retrospective Study
- Functional genomics identifies type I interferon pathway as central for host defense against Candida albicans
- Type III interferon is a critical regulator of innate antifungal immunity
- Interferon-gamma as adjunctive immunotherapy for invasive fungal infections: a case series
- Interferon‐γ as an Antifungal
- Therapeutic effectiveness of type I interferon in vulvovaginal candidiasis| Microbial Pathogenesis
- Recombinant Human IFNα-2b Response Promotes Vaginal Epithelial Cells Defense against Candida albicans| Frontiers in Microbiology
- The network interplay of interferon and Toll-like receptor signaling pathways in the anti-Candidaimmune response
- Type I Interferons Promote Fatal Immunopathology by Regulating Inflammatory Monocytes and Neutrophils during CandidaInfections
- Type I interferons during host–fungus interactions: Is antifungal immunity going viral?
- Anti-fungal role for type I IFN as dectin-1 triggers non-pathogenic TH17 cell development
- Facial Nerve Palsy as Complication in COVID-19 Associated Mucormycosis: A Case Series
- Vitamin D3 a new drug against Candida albicans
- Vitamin D-supplemented yogurt drink reduces Candida infections in a paediatric intensive care unit: a randomised, placebo-controlled clinical trial
- Влияние витамина D и интерферона α-2b на цитокиновый статус беременных с вагинальными инфекциями