Fungal infections are one of the complications of COVID-19. Mucormycosis is a fungal infection caused by the fungus Rhizopus oryzae in 70% of cases and develops in conditions of suppressed immunity. Mucormycosis affects 0.005 to 1.7 people per million population. The lethality rate is 46%.
The fungus Rhizopus oryzae is often found in soil, plant debris, spoiled food, and the upper respiratory tract of healthy individuals. The fungus causes mucormycosis when there are factors that predispose to immunodeficiency with reduced phagocyte activity – cells that absorb foreign particles.
Factors predisposing to mucormycosis include:
- Diabetes mellitus (60-80% of cases);
- tumor diseases of the blood;
- neutropenia caused by chemotherapy;
- Therapy with deferoxamine, a drug that binds iron and aluminum.
The most common form of mucormycosis is rhino cerebral (30-50% of cases). Diagnosing rhino cerebral mucormycosis in its early stages is challenging because the disease has no specific symptoms.
Symptoms of rhino cerebral mucormycosis:
- nasal congestion;
- unilateral headache behind the eye;
- swelling of the eye area;
- rarely, facial nerve palsy.
In patients with uncontrolled diabetes and mucormycosis, facial nerve palsy occurs in 11% of cases.
Also, facial nerve palsy is one of the complications of coronavirus, along with other neurologic symptoms, including:
- loss of sense of smell or taste;
- encephalitis;
- encephalopathy;
- cerebrovascular complications;
- myelitis;
- Guillain-Barré syndrome.
Facial Nerve Palsy in Coronavirus
American scientists have described the cases of three patients who developed facial nerve palsy with coronavirus and were found to have mucormycosis.
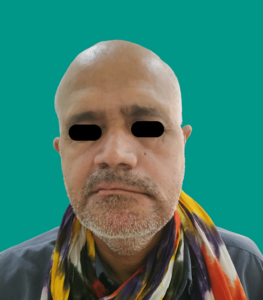
Patient 1
A 48-year-old man complained of swelling on the left side of his face for 20 days. The patient had previously been hospitalized for 15 days with COVID-19, and during treatment, the patient had an elevated blood glucose level of 351 mg/dL.
Examination revealed facial asymmetry and nerve palsy with involvement of the left side of the face. Clinical signs of facial nerve palsy included lowering the corner of the mouth, absence of wrinkles on the right side of the forehead, and incomplete closure of the right eye with the barely noticeable movement of the left side of the face.
Intraoral examination revealed necrosis of the mandibular bone and mobility of the mandibular teeth. MRI and histological examination showed purulent inflammation and mucormycosis of the tissues of the pterygopalatine fossa with spread to the parapharyngeal space.
Image source: https://www.cureus.com/articles/120611-facial-nerve-palsy-as-complication-in-covid-19-associated-mucormycosis-a-case-series#!/
Patient 2
A 50-year-old man complained of swelling on the left side of his face and blackish discharge from the left nasal cavity for 10 days. He had previously been diagnosed with diabetes mellitus during treatment with COVID-19.
Examination revealed facial asymmetry, unilateral facial nerve palsy on the left side, and soreness in the left suborbital and zygomatic areas. Signs of facial nerve palsy included drooping of the corner of the mouth, absence of wrinkles on the right side of the forehead, and incomplete closure of the right eye.
Computed tomography of the sinus cavities (CT scan) suggested acute fungal sinusitis and inflammation of the ocular adipose tissue. Histological examination confirmed mucormycosis of the rhino-orbital region.
Image source: https://www.cureus.com/articles/120611-facial-nerve-palsy-as-complication-in-covid-19-associated-mucormycosis-a-case-series#!/
Patient 3
A 43-year-old man complained of swelling on his face’s right side within one month. His medical history included controlled diabetes mellitus for one year and a recent hospitalization for COVID-19.
Examination revealed facial asymmetry and signs of unilateral facial nerve palsy, as well as pain on palpation of the right zygomatic region and mobility of the right upper first molar.
A CT scan of the PPH revealed sinusitis of the right maxillary sinus with an erosion of the sinus wall. In addition, soft tissue extending from the submandibular region to the right parotid space along the parotid duct and the neurovascular bundle was found. Histological examination confirmed mucormycosis.
Image source: https://www.cureus.com/articles/120611-facial-nerve-palsy-as-complication-in-covid-19-associated-mucormycosis-a-case-series#!/
Conclusion
COVID-19 is associated with a state of immunosuppression, which predisposes to fungal infection. Patients with coronavirus and uncontrolled diabetes mellitus have an increased risk of developing mucormycosis.
Risk factors for mucormycosis in coronavirus include:
- low oxygen levels;
- high glucose levels with diabetes as well as steroid treatment;
- a shift in acid-base balance to the acidic side;
- high iron levels;
- decreased phagocytic activity due to immunosuppression associated with coronavirus, steroid intake, or comorbidities;
- prolonged hospitalization with or without ventilators.
Mucormycosis may cause facial nerve palsy. Rhino cerebral mucormycosis may affect the pterygoid-facial fossa and spread to the facial nerve. In diabetic patients, facial nerve palsy may be associated with arterial pathology and impaired blood supply to the nerve.
Diabetes mellitus is associated with immunodeficiency. Hyperglycemia stimulates the fungus’s reproduction and reduces phagocytic activity, allowing the fungus to grow.
In the present study, mucormycosis, hyperglycemia, and recent coronavirus accompanied facial nerve palsy in three patients.
The initial site of infection was the pterygoid-femoral fossa. Widening of the pterygoid-facial fossa, visible on MRI, can be used to detect facial nerve involvement.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
Reference
Facial Nerve Palsy as Complication in COVID-19 Associated Mucormycosis: A Case Series