20-30% of patients with COVID-19 develop delirium and other mental disorders. With severe coronavirus, the risk of delirium increases to 60-70%.
Delirium is a state of confusion. With COVID-19, delirium indicates that the coronavirus has affected brain function.
Scientists from King’s College London have shown that when brain cells come into contact with blood taken from patients with COVID-19 with delirium, cell death increases and the formation of new brain cells, called neurogenesis, decreases. Violation of neurogenesis and death of neurons are possible reasons that patients with coronavirus experience a state of confusion, disorientation and difficulty remembering.
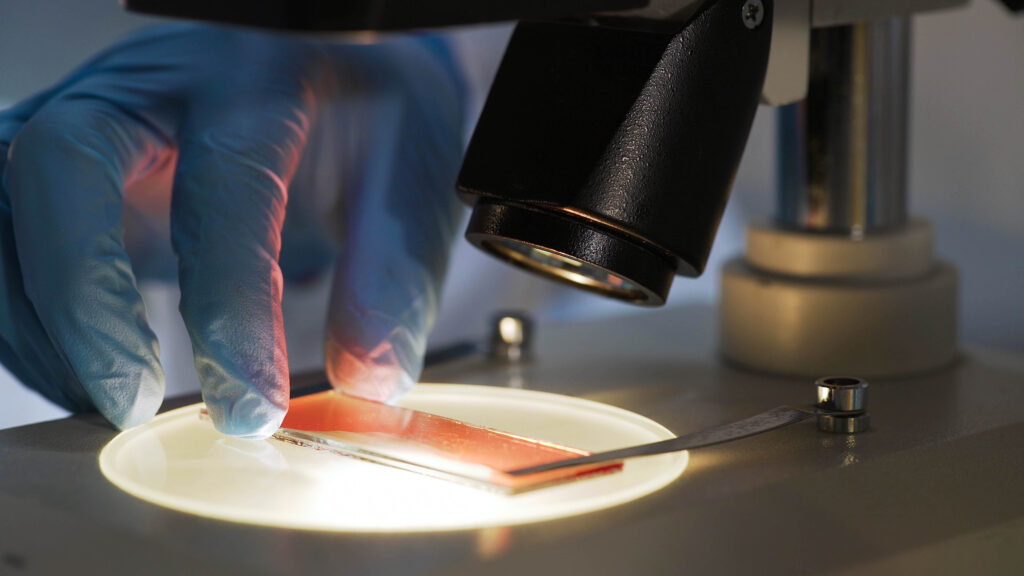
To understand the mechanisms by which the coronavirus disrupts neurogenesis, scientists collected blood samples from patients with COVID-19 suffering from delirium. The hippocampus cells, the part of the brain responsible for cognitive functions, including memory and learning ability, were treated with blood serum.
The blood serum of patients with delirium contained a higher level of the pro-inflammatory cytokine IL-6, compared with the serum of the control group with COVID-19 without delirium. When brain cells were treated with serum from patients with delirium, the levels of cytokines IL-12 and IL-13 increased in brain cells – this is how brain cells reacted to inflammation and an increase in the level of IL-6 in the body. Increased levels of IL-12 and IL-13 are associated with neurological disorders.
When the immune system overreacts to an infection, the body produces too many pro-inflammatory cytokines, which can penetrate from the blood into the brain, increasing the death of mog cells and disrupting neurogenesis. Therefore, the probability of delirium and other neurological symptoms increases with severe coronavirus.
The scientists tested their findings by treating hippocampal cells with an antibody against IL-6, preventing neuron death and impaired neurogenesis. Treatment of hippocampal cells with antibodies against IL-12 and IL-13 also protected neurons from death and prevented neurogenesis disorders.
Excessive immune system response to the coronavirus can lead to hyperinflammation and a life-threatening cytokine storm. To suppress the production of pro-inflammatory cytokines, patients with severe COVID-19 are prescribed Janus kinase inhibitors – baricitinib, ruxolitinib and tofacitinib.
In the present study, Janus kinase inhibitors reduced the level of IL-12 and IL-13 cytokines, restoring the normal viability of neurons and neurogenesis.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary: