Pregnant and lactating women were not included in any of the COVID-19 vaccine trials. So when health systems around the world began to vaccinate adults, the question arose for breastfeeding mothers: Should they be vaccinated against the coronavirus or not?
Pregnant women diagnosed with COVID-19 are more likely to be hospitalized than non-pregnant women of the same age. It may be since the body is under increased stress: due to the growth of the uterus, the capacity of the lungs decreases, and the immune system is suppressed so as not to harm the child. These factors do not disappear immediately after childbirth, so breastfeeding people are also susceptible to severe COVID-19.
The conclusion is obvious: pregnant and lactating women need additional protection from the SARS-CoV-2 coronavirus. However, questions remain: how does the vaccine work for pregnant and lactating women and how safe is it for the baby?
How Does The Coronavirus Vaccine Work on Pregnant and Lactating Women
American scientists tested the SARS-CoV-2 vaccine on a group of 131 women: 81 pregnant, 31 lactating and 16 non-pregnant. All participants were going to be vaccinated with one of two vaccines: Pfizer-BioNTech or Moderna. Scientists found that pregnant and lactating women generated the same robust antibody response as non-pregnant women. Antibody titers in response to the vaccine were significantly higher than in natural infection. The antibodies generated by the vaccine were present in all cord blood and breast milk samples. The level of IgG antibodies to SARS-CoV-2, but not IgA, increased in maternal blood and breast milk after the second dose of the vaccine.
How Safe is The Coronavirus Vaccine for A Baby When Breastfeeding?
Some medicines are not recommended during breastfeeding because they pass through breast milk and enter the baby’s body. For example, breastfeeding mothers are not advised to take high doses of aspirin, and even after taking low doses, the baby should be monitored for bruising and bleeding. Some vaccines are also prohibited for breastfeeding. The US Centers for Disease Control and Prevention (CDC) recommends that nursing mothers not receive the yellow fever vaccine. This vaccine contains a live, weakened form of the virus so the infection can be passed on to the baby.
However, COVID-19 vaccines do not contain live viruses. Therefore, unlike the yellow fever vaccine, COVID-19 vaccines cannot cause infection. In addition, it is implausible that COVID-19 vaccines will pass into breast milk. The fragile messenger RNA used in Pfizer-BioNTech and Moderna vaccines degrades so quickly that it cannot leave the cells it was injected into, let alone enter the bloodstream and breast milk.
Scientists from the University of California, San Francisco, USA, confirm this fact. The study involved six breastfeeding mothers who received one of the vaccines: Pfizer-BioNTech or Moderna. Participants provided breast milk samples 4-48 hours after vaccination. Vaccine safety testing found no trace of mRNA in breast milk in either case.
Antibodies in Breast Milk Protect The Baby from Infections
In young people, COVID-19 is often mild. However, coronavirus-infected babies under two years of age are more likely to be hospitalized than older children. The bronchioles (the passages through which air enters the lungs) are much smaller in infants. In addition, infants and children can develop multisystem inflammatory syndrome (MIS-C), a severe illness in which various body parts become inflamed after being infected with COVID-19.
Newborns up to 3-6 months do not develop antibodies against pathogenic bacteria and viruses. To protect the newborn’s body, breast milk is loaded with antibodies.
The mother’s immune cells B-lymphocytes constantly produce antibodies. Once lactation begins, the mammary glands send out a chemical signal that attracts these B cells to the breast. B cells are housed in glands and produce thousands of antibodies per second. These antibodies pass into breast milk in large quantities.
Unlike the molecules of drugs, coffee, and alcoholic beverages, which are so small that they can pass into breast milk on their own, antibodies are too large for this. Receptors on the surface of the milk ducts capture antibodies and pack them in protective fluid-filled vesicles that allow them to pass safely into the milk through the cells of the milk ducts.
The antibodies in breast milk do not enter the baby’s bloodstream but cover their mouth, throat, and intestines before being wholly digested. However, these antibodies provide protection.
Not all babies get breast milk. Research has shown that babies who were exclusively breastfed for the first six months had significantly fewer middle ear infections than babies who were breastfed for a shorter time or who did not receive breast milk at all. They also have a lower risk of respiratory tract infections. Furthermore, breastfeeding mothers who receive the flu vaccine and transmit protective antibodies to their babies through breast milk protect babies too young to be vaccinated.
Antibodies to Coronavirus are Found in Breast Milk After Suffering COVID-19 and Vaccination Against SARS-CoV-2
In early 2021, American researchers discovered that breast milk from people recovering from coronavirus contains antibodies to SARS-CoV-2. The study involved 18 women diagnosed with COVID-19. 76% of milk samples taken from women with COVID-19 had IgA antibodies to SARS-CoV-2, and 80% contained IgG antibodies to SARS-CoV-2.
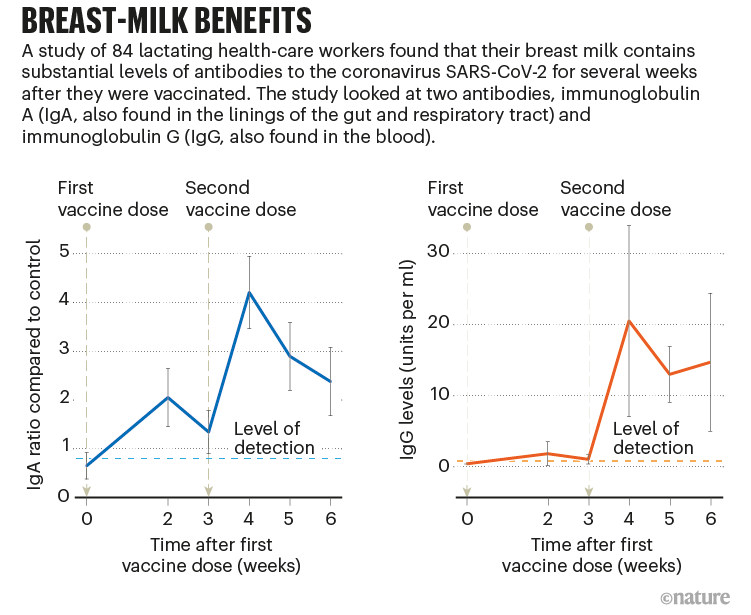
The presence of antibodies in breast milk after vaccination is also confirmed by Israeli scientists. The study involved 84 women. Study participants received 2 doses of Pfizer-BioNTech vaccine 21 days apart. Breast milk samples were collected before vaccine administration and once a week for 6 weeks, starting 2 weeks after the first dose.
Average levels of SARS-CoV-2 IgA antibodies in breast milk increased rapidly and significantly 2 weeks after the first vaccine when antibodies were detected in 61.8% of breast milk samples. At week 4, one week after the second vaccine, antibodies were detected in 86.1% of the samples. Average antibody levels remained elevated throughout the observation period. At week 6, 65.7% of the samples contained IgA antibodies to SARS-CoV-2.
IgG antibodies to SARS-CoV-2 remained low for the first 3 weeks. At week 4, their level rose to 20.5 U/ml when antibodies were detected in 91.7% of the samples. At weeks 5 and 6, 97% of the samples contained IgG antibodies to SARS-CoV-2.
The data are presented in the figure:
Changes in IgA and IgG levels in breast milk over time
Do antibodies from breast milk protect against coronavirus?
A research team from the Netherlands collected antibodies from people who had suffered a SARS-CoV-2 infection from breast milk. The study involved 38 nursing mothers with confirmed COVID-19. The control group consisted of 13 people. Scientists have discovered that antibodies from breast milk can neutralize the virus in the laboratory.
The American study of the beginning of 2021 confirms this result. 62% of breast milk samples could neutralize the SARS-CoV-2 coronavirus in the laboratory, while milk samples collected before the COVID-19 pandemic could not do this.
Israeli scientists have also found that antibodies in breast milk formed after vaccination neutralize the coronavirus. The study involved 10 nursing mothers who received two doses of the Pfizer – BioNTech vaccine. The formation of antibodies was rapid and highly synchronized between breast milk and serum, reaching stabilization 14 days after the second dose of the vaccine. The predominant serum antibodies were IgG. Breast milk contained both IgG and IgA with a neutralizing ability.
Side effects of vaccination during breastfeeding
Israeli scientists have evaluated the possible side effects of the Pfizer-BioNTech vaccine in nursing women and their babies. In addition to breast milk samples, the study participants filled out weekly questionnaires about their well-being and the side effects associated with vaccination. No mother or infant experienced any severe side effects during the study period. 47 women out of 84 (55.9%) reported vaccination-related side effects after the first dose and 52 (61.9%) after the second dose of the vaccine. The most common complaint was pain at the injection site. Four infants had fever during the study period 7, 12, 15 and 20 days after the mother’s vaccination. All had upper respiratory tract infection symptoms, including cough and congestion, which disappeared without treatment, except one child hospitalized for evaluation of neonatal fever due to his age and was treated with antibiotics until the culture results were received. No other side effects have been reported.
How Long Antibodies Remain in Breast Milk After Vaccination?
A study involving 33 people showed that the production of antibodies in adults who received the Moderna vaccine lasts at least 6 months. It may mean that babies will receive protective antibodies from breast milk six months after the mother’s vaccination, although the concentration of antibodies in breast milk decreases over time.
The antibodies are digested in the baby’s intestines after a few hours or days. It means that after stopping breastfeeding, passive immunity will disappear. Feeding breast milk to older children will also not be able to provide long-term immunity. Therefore, even for exclusively breastfed infants, doctors urge mothers to continue to follow public health strategies when visitors come to them: anyone who communicates closely with an infant should wear a mask and be vaccinated.
Conclusions
After vaccination, IgA and IgG antibodies to SARS-CoV-2 are consistently detected in breast milk. IgA antibodies are present in milk as early as 2 weeks after vaccination. The spike in IgG levels occurs after 4 weeks, a week after the second vaccine. Antibodies produced after COVID-19 are also present in breast milk. Both these and other antibodies showed a neutralizing effect in the laboratory. It means that the antibodies contained in breast milk can potentially protect infants from the SARS-CoV-2 coronavirus. Therefore, the World Health Organization recommends that mothers continue to breastfeed after vaccination.
Sources
- COVID vaccines and breastfeeding: what the data say
- SARS-CoV-2–Specific Antibodies in Breast Milk After COVID-19 Vaccination of Breastfeeding Women
- Characterization of SARS-CoV-2 RNA, Antibodies, and Neutralizing Capacity in Milk Produced by Women with COVID-19