China
From January 29 to April 30, 2020, specialists from the Chinese Academy of Medical Sciences studied reinfection (reinfection) with coronavirus – these are cases when viral genomes are different. Scientists have confirmed reinfection in 2% of study participants. In half of these cases, reinfection occurred when the patients had high levels of antibodies in the blood, considered protective by the scientific community. The range of times for reinfection was from 19 to 57 days after the end of the primary infection. Details of the study are published in the National Science Review.
Study Details
The study involved 273 people with COVID-19. It is 46% of cases reported during the same period in Beijing, China. None of the participants had autoimmune diseases, cancer, or immunosuppressive drugs.
Scientists tracked clinical and laboratory data during hospitalization and followed these patients after they were discharged. During the first case of the disease, specialists decoded the genome of the coronavirus isolated from the blood of each patient. In the next episode of COVID-19, scientists also decoded the genome of the coronavirus and compared it with the genome in the first case. If the genomes were significantly different, this fact was recorded as a reliably established repeated coronavirus infection.
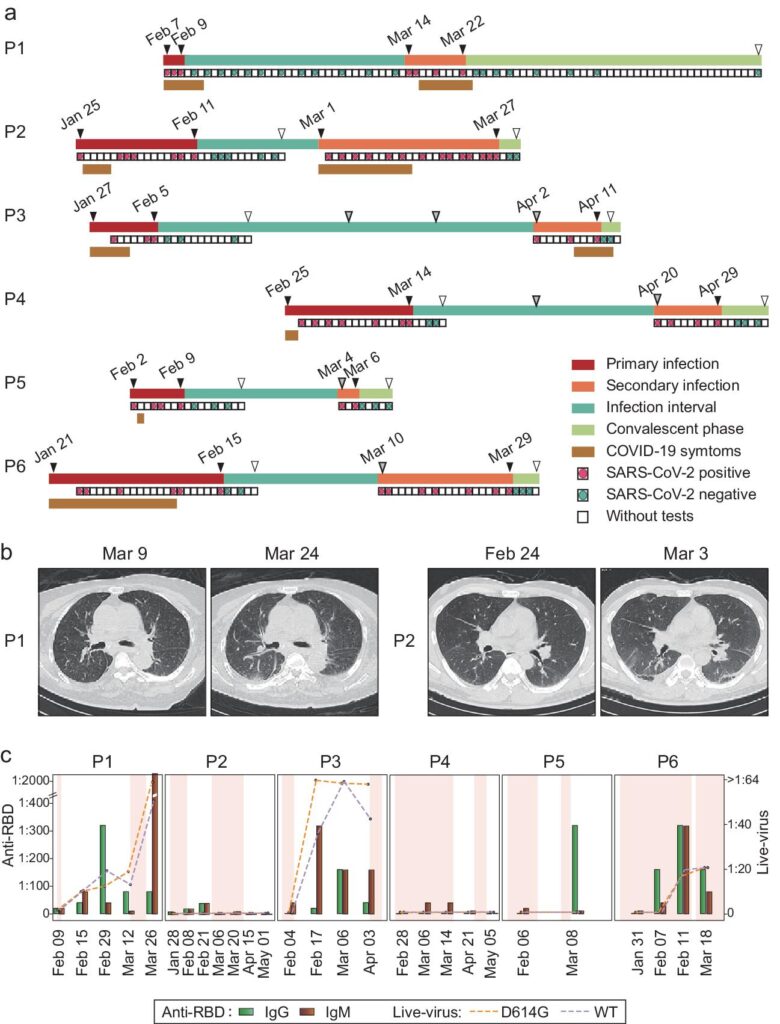
As a result, a repeat episode of COVID-19 was reliably confirmed in 6 study participants. Five participants – adults from 33 to 84 years old, one – two years old child. Chronology of the disease, dynamics of the titer of neutralizing activity of antibodies:
Designations in the figure “a” – the chronology of the disease:
- red – primary infection;
- orange – reinfection;
- blue – the course of the disease;
- green – convalescence phase;
- brown – symptoms of the disease were registered;
- red square – a positive test for coronavirus;
- blue square – a negative test for coronavirus;
- white square – no coronavirus test has been performed.
Designations in figure “c” – titer dynamics and neutralizing activity of antibodies:
- green bars – IgG titer;
- brown bars – IgM titer;
- orange line – neutralizing activity of antibodies against authentic SARS-CoV-2 virus (wild type);
- purple line – neutralizing activity of antibodies against the D614G line of the SARS-CoV-2 virus.
Source: https://academic.oup.com/view-large/figure/267766211/nwab006fig1.jpeg
Patients P1, P3, P6 had a high level of antibodies at the time of reinfection. At the same time, a level exceeding 1: 100 is recognized by the world scientific community as protecting against infection.
Clinical picture and test results of patients with repeated coronavirus infection:
| Р1 | Р2 | Р3 | Р4 | Р5 | Р6 | |
| Sex | F | M | M | M | F | M |
| Age | 84 | 33 | 59 | 33 | 2 | 74 |
| Disease severity | Critical | Moderate | Moderate | Moderate | Moderate | Critical |
| Accompanying illnesses | Hypertension, heart disease | No | No | No | No | Hypertension, coronary heart disease |
| Interval between episodes (days) | 33 | 19 | 57 | 35 | 22 | 24 |
| 1st case Symptoms | Fatigue, cough, shortness of breath | Fever | Fatigue, cough, sore throat, nasal congestion | Fever | Fever, cough | Fever, fatigue, cough, shortness of breath |
| 2nd case Symptoms | Fever | Fever, cough, shortness of breath | Fatigue, cough, nasal congestion | No | No | No |
| 1st case Hospitalization | 88 (total) | 30 | 20 | 21 | 16 | 26 |
| 2nd case Hospitalization | 88 (total) | 28 | 12 | 16 | 7 | 23 |
| 1st case Antiviral drug intake | No | Interferon, lopinavir-ritonavir | No | Interferon, lopinavir-ritonavir | Interferon | Interferon |
| 2nd case Antiviral drug intake | No | Ribavirin | Interferon | Interferon, lopinavir-ritonavir | Interferon | No |
USA
In North America, the first confirmed case of COVID-19 reinfection was reported on April 18, 2020, in Nevada in a 25-year-old man. The man had no concomitant diseases and signs of suppressed immunity.
The patient developed symptoms on March 25, 2020: sore throat, cough, headache, nausea, diarrhea. Hospitalization was not required. Symptoms disappeared on April 27, 2020. Two subsequent negative coronavirus tests showed no infection.
Reinfection occurred on May 28, 2020, when the man again showed symptoms of COVID-19: fever, headache, dizziness, cough, nausea, diarrhea. The second case was more severe than the first: the patient was hospitalized with hypoxia and shortness of breath. The chronology of the disease is shown in the figure:

The analysis showed a significant difference in the genomes of the coronavirus in the first and second cases. To confirm the point of reinfection, specialists used two different methods and received the same result.
The details of the study are published in The Lancet.
Ecuador
The first confirmed case of COVID-19 reoccurrence occurred in Ecuador on May 12, 2020. A 46-year-old man suffered from weakness and severe headaches. His wife and daughter had the same symptoms. PCR analysis revealed infection with coronavirus. After 21 days, repeat PCR tests for coronavirus were negative.
Reinfection was registered on July 20, 2020. Symptoms of the disease were more severe than in the first case: temperature 38.5 ° C, severe chest pain, shortness of breath, nasal congestion. Hospitalization was required. Radiography revealed pneumonia.
The decoding of the viral genomes in the first and second cases revealed a significant difference. In the first case, the genome was assigned to the B1.p9 line, and in the second, to A.1.1.
The study is published on the website of the Social Science Research Network
Conclusions
Reinfection with COVID-19 occurs in ~ 2% of cases. High levels of neutralizing antibodies and a previous severe form of the disease were found in 1% of reinfection episodes. Reinfection can occur within a month after recovering from primary COVID-19.
Clinically, reinfection may be more severe than primary COVID-19. Scientifically confirmed cases of reinfection have been reported in people of all ages: from 2 to 84 years old.
Sources
- COVID-19 reinfection in the presence of neutralizing antibodies
- Genomic evidence for reinfection with SARS-CoV-2: a case study
- COVID-19 Re-Infection by a Phylogenetically Distinct SARS-CoV-2 Variant, First Confirmed Event in South America