The humoral immune response plays a crucial role in protecting a person from viral infection. Humoral immune responses are usually characterized by primary IgM antibody responses, followed by secondary antibody responses associated with immune memory and consisting of IgG, IgA, and IgE.
French scientists have studied that in coronavirus infection, the first antibodies of the IgA isotype appear.
Studying the dynamics of IgA antibodies
Scientists from leading French universities measured the humoral immune responses of patients with varying degrees of COVID-19 severity. The researchers studied the neutralizing potential of antibodies in the upper respiratory tract’s mucosa, lungs’ secretions, and blood serum.
The study results showed that IgA antibodies are often detected before the appearance of IgG and IgM antibodies, and the neutralizing activity of IgA is the highest. Scientists suggest that IgA antibodies play a vital role in the early neutralization of the virus.
Research design
The study was conducted at the Medical Center of the Sorbonne University in Paris. The study involved 159 patients with confirmed COVID-19. The control group consisted of 20 healthy donors of the same age and gender.
All participants had their biological material collected and analyzed regularly for 1 month. The studied biochemical parameters:
- The number of plasmablasts (cells that produce antibodies). The plasmablasts’ calculation was performed separately for each type of produced antibodies: IgG, IgA, IgM.
- Titer (number) of antibodies in the blood serum: IgG, IgA, IgM.
- Comparison of the neutralizing activity of antibodies types IgG and IgA.
Plasmablasts population
Plasmablasts are highly specialized cells formed from B-lymphocytes. One plasma cell produces only one type of antibody. The rapid appearance of plasmablasts in the peripheral blood is a feature of the acute phase of viral infections.
Dynamics of plasmablasts
In patients with COVID-19, the proportion of plasmablasts in the total B-cell population increased rapidly from day 1 to day 9 from the onset of symptoms. The peak amount was reached between 10 and 15 days. Then there was a decrease in the proportion of plasmablasts:
|
Days from the onset |
Plasmablasts in |
Plasmablasts |
|
1 – 9 |
4.9% |
0.5% |
|
10 – 15 |
11.8% |
0.5% |
|
16 – 25 |
4.4% |
0.5% |
|
50 |
0.5% |
0.5% |
All calculations were performed by flow cytometry (piece-by-piece analysis).
Quantitative distribution of plasmablasts producing different types of antibodies
Scientists have made a quantitative assessment of early (1 – 9 days) immune response to coronavirus infection.
The largest population of plasmablasts produced IgA antibodies. Their share in the total number of plasmablasts was 61.4% on average in all patients. The second-largest number were plasmablasts that produce IgG antibodies – 27.9%. IgM antibodies were produced by a small number of cells – 10.5%.
Among the IgA antibodies, IgA1 subclass antibodies predominated – 66%, and IgA2 subclass antibodies – 31.6%.
|
Antibodies-producing |
Plasmablasts that |
|
IgA |
61.4% |
|
IgG |
27.9% |
|
IgM |
10.5% |
The measurements were carried out by intracellular staining.
The first wave of circulating IgA plasmablasts peaked between 10 and 15 days after the onset of symptoms. The second wave is IgG plasmablasts. They were dominant on day 22.
The number of peripheral IgM plasmablasts did not change significantly at the early stage of the disease and only slightly increased later.
Distribution of plasmablasts in tissues
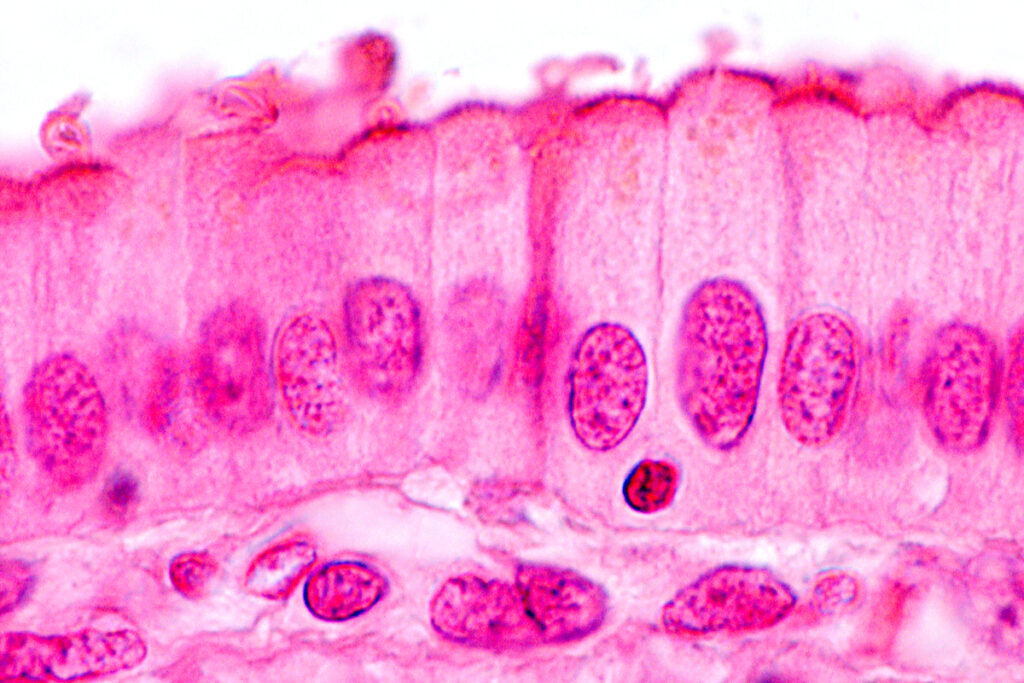
The researchers analyzed the circulating plasmablasts for the surface chemokine receptor (CCR10), promoting immune cells’ migration into the mucous membranes. This receptor leads cells most often to the lungs.
It was found that less than 10.9% of memory cells and naive B-lymphocytes possess this receptor. Among the plasmablasts, there were 34.9% of them.
Detailed analysis of plasmablasts revealed that the chemokine receptor CCR10 was present in 60.5% of IgA plasmablasts and 23.3% of IgG plasmablasts. This distribution corresponds to the characteristics of plasmablasts that are found in the mucosa of patients. Scientists also suggest that IgG plasmablasts predominate in other organs, for example, in the bone marrow.
| Antibodies-producing plasmablasts |
Plasmablasts migrating to the mucous membranes |
|
IgA |
60.5% |
|
IgG |
23.3% |
Features of the IgA, IgG, IgM antibody response
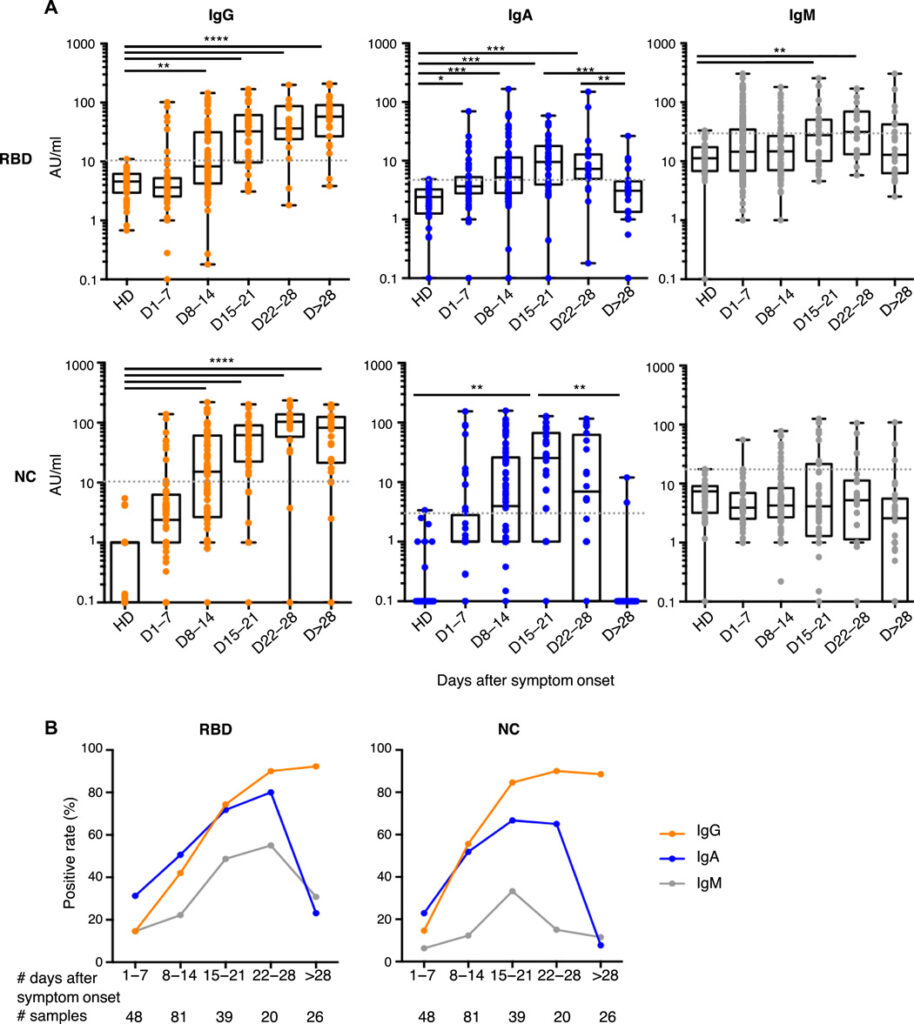
The researchers evaluated the prevalence of IgA, IgG, and IgM antibodies that recognize the coronavirus nucleocapsid protein (NC) or spike receptor-binding domain (RBD) in the serum samples of 132 patients with COVID-19:
Source: https://www.science.org/doi/10.1126/scitranslmed.abd2223
To do this, the researchers used an enzyme-linked immunosorbent assay to measure the level of antibodies to several antigens at the same time.
It was found that in the first 7 days from the onset of symptoms of the disease
IgA to RBD antibodies appeared in 31% of cases, and IgG to RBD-in 15%.
At the same time, the number of antibodies to NC was the same for all isotypes.
A similar analysis, performed at several time points, showed that IgA antibodies to RBD appear in patients with COVID-19 earlier than IgG antibodies:
|
Spike receptor-binding domain (RBD) |
Range of days |
|
IgA |
3 – 24 |
|
IgG |
8 – 24 |
Scientists suggest that for the early diagnosis of COVID-19, an analysis for IgA antibodies to the coronavirus can be used.
The proportion of patients with IgG to RBD gradually increased and became stable by about the fourth week after the onset of symptoms. The reverse pattern was observed in patients with IgA to RBD: the peak occurred on day 22, and then the number gradually decreased by day 28:
|
Days from the onset |
Patients with |
Patients with |
| 1 – 7 | 31% | 15% |
| 8 – 14 | 51% | 42% |
| 15 – 21 | 72% | 74% |
| 22 – 28 | 80% | 90% |
| > 28 | 23% | 92% |
Similar kinetics was observed in IgG antibodies to the nucleocapsid protein (NC).
IgA-NC antibodies quickly disappear 1 month after the onset of symptoms and do not appear again.
The traditional marker of acute infection-IgM antibodies was detected only in 7 of the 48 early samples. Moreover, IgM-NC antibodies were detected in only one case.
In two patients, antibodies of all isotypes were no longer detected on day 32 and 47, respectively.
Titers of antibodies to fragments of the coronavirus
The titers of IgA and IgG antibodies to RBD and NC increased over time:
| Days from the onset of symptoms |
RBD Titres, U/ml |
NC titers, U/ml |
| 1 – 7 | 3.6 | 2.4 |
| 8 – 14 | 8.3 | 15.2 |
| 15 – 21 | 32.6 | 61.7 |
| 22 – 28 | 36.5 | 103.5 |
The relationship between the presence of antibodies and the severity of COVID-19
The researchers analyzed early blood serum samples obtained no later than 10 days after clinical symptoms appeared.
- Criteria for the severity of the disease included:
- Transfer to the intensive care unit.
- Oxygen therapy above 5 liters per minute.
- Artificial ventilation of the lungs.
- Acute renal failure.
- Death.
It was found that the appearance of early virus-specific antibodies IgA, IgM, IgG did not significantly differ in patients with different degrees of severity.
Neutralizing activity of the antibodies IgA, IgG
The researchers sought to assess each IgA and IgG isotypes’ contribution to the virus’s neutralization. Samples for analysis were collected between 6 and 24 days after the onset of symptoms.
It was found that at an early stage of infection, IgA has a more tremendous potential to neutralize the virus than IgG.
The exception was 2 patients who had low IgA levels, but an early IgM response was detected.
The neutralization potential was associated only with IgA to RBD, and the neutralization efficiency increased with an increase in the titer of this type of antibody.
The researchers note that IgG is 5 times more common in serum than IgA, but IgA is approximately 7 times more effective.
Conclusion
By their nature, IgA antibodies were more neutralizing at an early stage of COVID-19 than IgG. The high prevalence of IgA in the mucous membranes helps reduce the viral load in the most affected organs and reduce the rate of infection in people.
The number of IgA antibodies gradually decreases within 1 month of the onset of symptoms. Further, IgG antibodies begin to play a significant role in antiviral protection and the formation of immunity.
Source
IgA dominates the early neutralizing antibody response to SARS-CoV-2