People with Down syndrome have an increased risk of complications from COVID-19:
- Patients with Down syndrome require more extended periods of hospitalization and mechanical ventilation.
- Among those hospitalized with coronavirus, 83.3% of patients with Down syndrome developed sepsis, while patients without Down syndrome developed sepsis in only 46.7% of cases.
- After hospitalization with coronavirus, 25% of patients with Down syndrome died. Of patients without Down syndrome, only 6.7% died.
What Factors Affect The Severity of COVID-19
Down syndrome is a genetic disease caused by a partial or complete third copy of the 21st chromosome instead of the usual two copies.
Chromosome 21 contains several genes that play a crucial role in innate and adaptive immunity. Among them are genes encoding interferon receptors of types I, II, and III.
Due to the third copy of the 21st chromosome in people with Down syndrome, the expression of interferon receptors is increased, as well as the concentration of type I interferons in plasma. Therefore, the immune cells of people with Down syndrome are 3-7 times more sensitive to interferon signals.
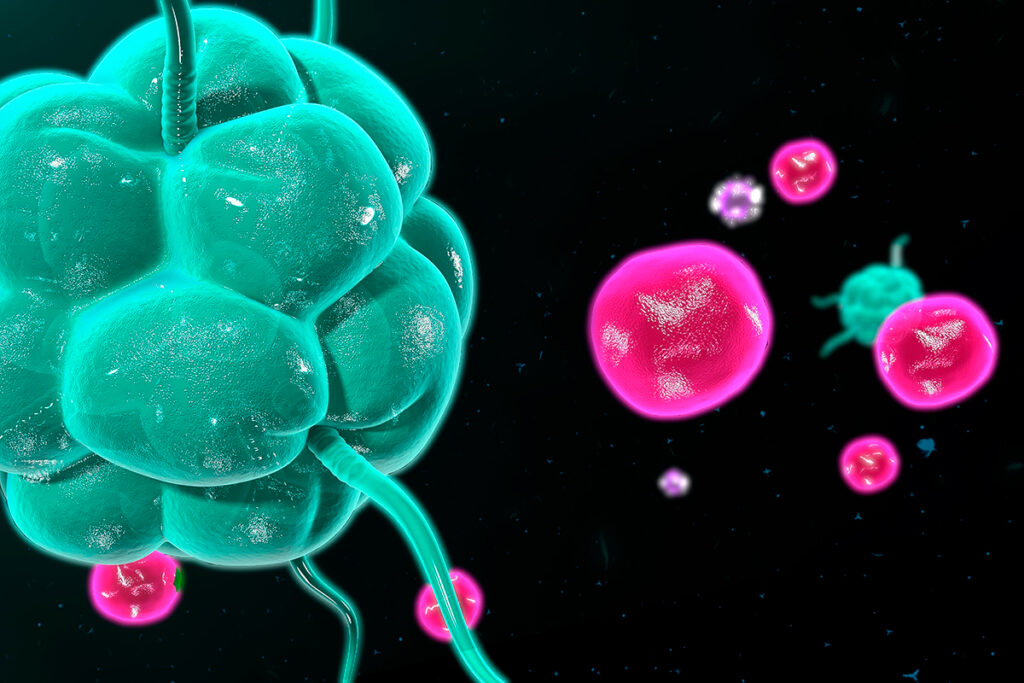
A more intense interaction of interferons with their receptors triggers an antiviral response of innate immunity. It would seem that this response should better protect against viral infections. However, people with Down syndrome develop a more severe disease after infection with coronavirus.
When interferons bind to their receptors on the surface of cells, the expression of interferon-stimulated genes (ISGs) is triggered, suppressing the virus. Monocytes from people with Down’s syndrome express higher levels of ISG than monocytes from healthy people. This chronic immune activation has been observed in HIV patients and has led to immune dysfunction.
Constant activation of the interferon system can lead to a deterioration in immune responses to infections and the development of autoimmune diseases. Causes of immunosuppression:
- The activity of PD1, TIM3, and LAG3 receptors on the surface of T cells increases with chronic activation of the interferon system. These receptors impair adaptive immune responses, leading to aging and a depleted immune system.
- Interferon signaling increases levels of the pro-inflammatory cytokines and chemokines IL-6, IL-22, CCL2, TNF, and VEGFA. In the plasma of people with Down syndrome, their levels are elevated, which leads to increased inflammation.
- Immune system dysfunction is also associated with increased NK and killer T cells and decreased B cells.
In addition, people with Down syndrome have increased levels of ACE2 and TMPRSS2 proteins, with which the coronavirus enters the cell. Continuous activation of the interferon system enhances ACE2 expression in lung epithelial cells. At the same time, TMPRSS2 is encoded on chromosome 21, so people with Down syndrome have a threefold increase in TMPRSS2 expression. All this makes people with Down syndrome more susceptible to coronavirus.
Treatment and Vaccination Against COVID-19
People with Down syndrome have a normal antibody response after being vaccinated against the coronavirus. However, the response to some vaccines in people with Down syndrome is reduced. American scientists investigated the response to the seasonal influenza vaccine and the pneumococcal polysaccharide vaccine in children with Down syndrome. The mean serum IgG antibody levels in these children were significantly higher than in healthy controls. However, children with Down syndrome had a significantly lower number of T-helper cells. T helper cells are essential for adaptive immunity. They enhance the activity of other immune cells, in particular, cytotoxic ones. Also, T-helper cells are required for antibody class switching. In addition, the number of B-cells and T-memory cells was reduced in children with Down syndrome, and antibody class switching was less effective.
People with Down syndrome have elevated baseline levels of inflammation. Higher levels of inflammation and increased levels of pro-inflammatory innate immune cells are associated with poorer responses to vaccination.
This data means that the duration of protection after being vaccinated against coronavirus in people with Down syndrome may be shorter.
Baricitinib may reduce baseline inflammation in people with Down syndrome. Baricitinib is a Janus kinase (JAK) 1/2 inhibitor that blocks interferon signaling and has anti-inflammatory and immunosuppressive properties. Pre-treatment with baricitinib may restore immune system function and the ability to sustain antibody responses to vaccines.
In addition, baricitinib is used to treat severe COVID-19. Baricitinib reduces the cytokine storm and reduces the penetration of coronavirus into cells.
Post-COVID Syndrome
The risk of post-COVID syndrome is increased by:
- prolonged hospitalization;
- a large number of comorbidities;
- worsening of symptoms during the first week of illness;
- the presence of autoantibodies.
People with Down’s syndrome may develop post-COVID syndrome because these people often require long-term hospitalizations and have comorbidities such as diabetes, obesity, cardiovascular disease, and secondary infections.
Conclusion
Genetic and cellular disorders in people with Down syndrome may increase the risk of severe COVID-19. A third copy of the 21st chromosome enhances coronavirus’s penetration into cells, contributing to chronic inflammation and dysfunction of T-cells and B-cells. Together with comorbidities, these factors predispose to a more severe course of the coronavirus.
Chronic inflammation is associated with constant activation of the interferon system. Exposure to the interferon system during coronavirus infection may reduce inflammation, restore immune function, and reduce the severity of COVID-19.
Useful article, necessary information? Share it!
Someone will also find it useful and necessary:
References
- COVID-19 and Down syndrome: the spark in the fuel
- Immune evaluation and vaccine responses in Down syndrome: Evidence of immunodeficiency?