Immunity protects the body from foreign microbes and molecules – this is the traditional view. However, the immune system also responds to changes in self-regulation and disruption of the integrity of organs and tissues-it detects potential danger and activates protective mechanisms.
Cancer cells and cells transformed by foreign pathogens (for example, human papillomavirus, hepatitis B and C viruses, Epstein-Barr virus, human T-lymphotropic virus I, herpes virus associated with Kaposi’s sarcoma, and Helicobacter pylori) are genetically different from normal cells and, like virus-infected cells, emit signals to which the immune system responds. These signals are called damage-related molecular patterns (DAMP). They contribute to establishing an effective and long-lasting immune response that allows the destruction of virus-infected cells because they express virus-encoded proteins and tumor cells because they express tumor-associated antigens – TAA. Antiviral and antitumor immune responses share common DAMP, including type I interferons.
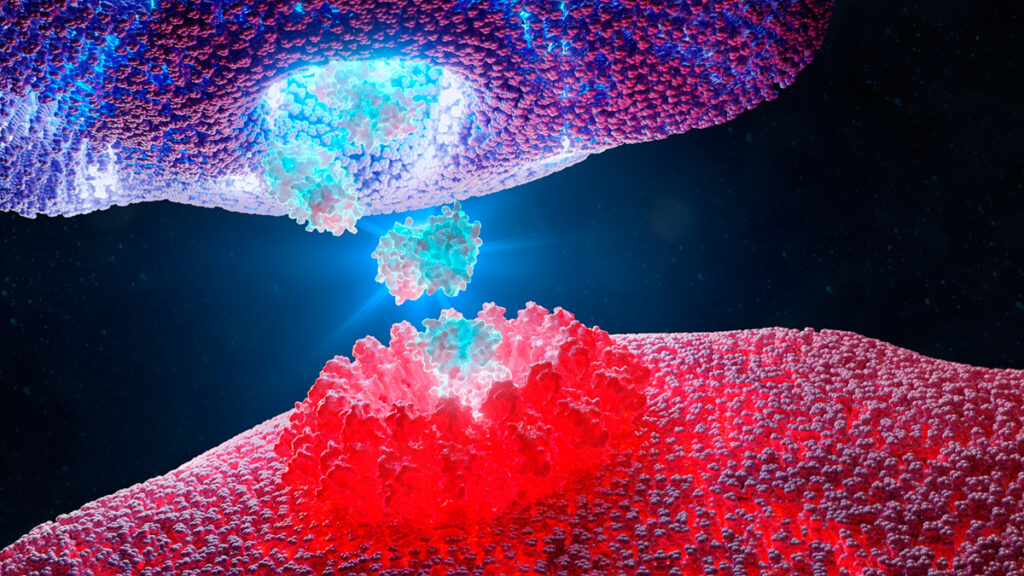
Interferons (IFN) are signaling molecules produced and perceived by almost all cell types in the body. Interferons are the link connecting innate and acquired immunity.
According to their general biological properties, cellular source, genetic structure, and the receptor through which they transmit the signal, IFNs are divided into three families: Type-I, Type-II, and Type-III. In humans, type I IFN consists of 13 proteins-cytokines IFN-α, one IFN-β, and several yet-to-be-characterized products of a single gene (IFN-ε, IFN-τ, IFN-κ, IFN-ω, IFN-δ, and IFN-ζ).
Almost all cells in the body can produce type I IFN after recognizing pathogen-associated molecular structures (PAMP) – foreign and native nucleic and non-nucleic acids. The cell recognizes PAMP using pattern recognition receptors (PRR). IFN-I binds to the IFNAR interferon receptor and triggers the transcription of several hundred IFN-stimulated genes (ISG) that control the immune cell response.
During infectious and cancer diseases, the production of IFN-I signaling molecules is tightly regulated. It ensures that the strength and duration of the immune response will be adequate but will not cause tissue damage and autoimmune reactions due to excessive long-term signaling. Each of the IFN-I subtypes induces a unique and partially overlapping set of ISGS that can act at different stages of the virus and cancer life cycle.
Interferon type I in cancer
IFN-I can have anti-and pro-oncogenic effects, acting directly on tumor cells and indirectly on immune infiltrating cells.
Internal effects: IFN type I affects cancer cells
The intrinsic efficacy of type I IFN for cancer cells depends on specific cellular effects, such as growth suppression, triggering apoptosis( cell death), differentiation, migration, altering the expression of tumor-associated antigens (TAA) on the cell surface, and stimulating the epithelial-mesenchymal transition.
IFN-I affects different phases of the mitotic cell cycle – the processes from cell formation to cell division. G1 is the phase of the mitotic cycle, during which the cell increases in size and synthesizes mRNA and protein, which are needed for DNA synthesis. The next step is the S-phase, during which the cell doubles the chromosomes and centrosomes. Most often, IFN-I blocks the cell cycle in the G1 phase.
The role of type I IFN in suppressing tumor growth. Research has shown that:
- In vitro treatment of human breast cancer cell lines with exogenous crude IFN-I drugs has a direct antiproliferative effect associated with cell cycle prolongation.
- IFN-α inhibits the growth of human prostate cancer cells and mouse macrophages, delaying the transition from G1 to S phase due to increased expression of the cyclin-dependent kinase (CDKN)1A inhibitor, best known as p21.
- IFN-I induces other CDK inhibitors, including CDKN1B and CDKN2B (most commonly known as p27 and p15, respectively), whose overregulation leads to cell cycle blockage G1 phase.
- In human colon cancer cells, the antiproliferative effect of IFN-I is based on the p21-dependent prolongation of the S-phase rather than on the cell cycle blockade in the G1 phase.
The opposite experimental data show that IFN-I can either cause tumor cells’ death or protect cancer cells from chemically induced cell death – apoptosis. This discrepancy may be related to the degree of cellular differentiation, factors associated with the tumor, and differences in the tumor microenvironment.
The introduction of type I IFN regulates two primary apoptotic responses: the external pathway or the death receptor-mediated pathway and the internal or mitochondrial pathway. The outer path requires activation of cell death receptors, whereas the internal way involves releasing apoptosis factors from mitochondria.
IFN-β enhances the expression of human leukocyte antigen (HLA) class I and regulates the antigenic landscape of cultured melanoma cells. IFN-β simultaneously increases TAA and HLA Class I, thus improving immune recognition and cytotoxic destruction of tumor targets, respectively.
The epithelial-mesenchymal transition (EMT) is when epithelial cells lose their polarization and intercellular contacts and change shape, becoming similar to connective tissue cells. Cancer cells that have undergone EMT can migrate to other organs and tissues, which leads to tumor metastasis. Such cells acquire the property of stemness – the ability to self-renew and divide – and resistance to drugs. Cancer stem cells are the driving force behind tumor recurrence.
The role of type I IFN in stimulating tumor growth. Research has shown that:
- IFN-α-induced protein 27 promotes epithelial-mesenchymal transition and leads to ovarian cancer. In this study, this phenomenon led to the emergence of drug-resistant cells with the phenotype of cancer stem cells.
- IFN-I signaling has the potential to contribute to the generation and/or maintenance of cancer stem cells. IFN-α affects migration and invasion of pancreatic duct adenocarcinoma cells by activating specific markers of cancer stem cells, such as CD24, CD44, and CD133.
- Stimulation of the TLR3 pattern recognition receptor on somatic cells causes global changes in the expression of epigenetic modifiers, which lead to enhanced chromatin remodeling, nuclear reprogramming, cell plasticity, pluripotency, transdifferentiation, and even malignant transformation. Toll-like receptors (TLRs) are highly expressed in cancer cells and are associated with poor prognosis. Experiments on breast cancer cells have shown that the stimulation of TLR3 by simultaneous transmission of NF-kB and β-catenin signals contributes to enriching the subpopulation of cells with the phenotype of cancer stem cells.
- In hematopoietic stem cells and progenitor cells, chronic IFN-I stimulation resulted in the loss of resting-state and cellular dysfunction. That was due to the accumulation of reactive oxygen species under the influence of IFN-I.
- In cancer cells, IFN-I activated the PD – L1 protein, a ligand of programmed death. PD-L1 is a cell surface molecule that is expressed by most tumor cells. This molecule triggers signals that suppress cytotoxic T-lymphocytes, depleting them, and thus plays an essential role in evading cancer from the immune system.
It is tempting to suggest that a sustained therapeutic response may depend on a combination of type I interferon therapy or Type I IFN-inducing therapy with antibodies targeting the PD1-PD-L1 axis. The scientists demonstrated that the oncolytic vesicular stomatitis virus, designed for the constant expression of IFN-β, had significant anti-leukemia activity, which was further enhanced when combined with an antibody against PD-L1.
External effects: IFN type I affects the immune cells that destroy the tumor
In addition to the direct effect on cancer cells, IFN-I has an external impact on tumors, regulating the immune response and suppressing the formation of new blood vessels (angiogenesis). Angiogenesis slows down due to the suppression of vascular endothelial growth factor (VEGF) expression and impaired proliferation and migration of endothelial cells.
Although the immune system plays a vital role in deterring cancer development, it can also contribute to the appearance of tumors not controlled by the immune system. According to the immune editing model, malignant cells initially contained through immune surveillance can grow into clinically expressed tumors, provided that:
- they stop expressing the proteins that make them recognizable to the cells of the immune system (immune selection);
- they actively counteract immune responses (immune suppression).
Cancer immune reduction is a process in which the immune system protects the body from the development of a tumor and promotes the growth of tumors with reduced immunogenicity, that is, the ability of a foreign substance to cause an immune response. Cancer immune reduction consists of three stages:
- at an early stage, malignant cells are recognized and destroyed by immune effector cells (elimination);
- at a later stage, small tumors are still held back by increasingly less effective immune responses (equilibrium);
- finally, neoplastic cells lose their antigenic properties or create robust immunosuppressive networks, thus avoiding any control (escape).
Type I interferons are involved in all three phases. Endogenously produced IFN-I is necessary for immunocompetent mice to reject highly immunogenic sarcomas caused by exposure to the carcinogen 3-methylcholanthrene (MCA) and prevent the growth of primary tumors caused by carcinogens. Several MCA-induced sarcomas from mice without the type I interferon receptor (Ifnar1-/-) were rejected in a T-cell-dependent manner in wild-type mice. It suggests that tumors that occur in the absence of an IFN-I response are more immunogenic than tumors that grow in organisms with IFNAR.
Type I interferons can stimulate external antitumor effects. When mixed IFN drugs were administered to mice with lymphocytic leukemia, survival rates increased regardless of whether the tumor cells themselves were initially sensitive to the antiproliferative effect of these IFN drugs.
Studies in mice and humans have uncovered many mechanisms by which IFN-I acts on immune cells, triggering a solid antitumor response:
- Highly metastatic Friend leukemia cells, genetically modified to secrete IFN-α1, show a marked loss of their carcinogenic potential when administered to immunocompetent mice and inhibit the growth of metastatic parent cells in transplant assays, mainly by CD8+ cytotoxic T-lymphocytes.
- IFN-α induced dendritic cell differentiation/activation in mice and humans and stimulated new immunotherapy regimens. Dendritic cells are intermediaries between innate and acquired immunity. They are involved in the antigen presentation process-presenting foreign molecules to T-lymphocytes to trigger an immune response.
- IFN-I combines innate and acquired immunity. IFN-I stimulates the production of various cytokines (TNF, IL-1, IL-6, IL-8, IL-12, and IL-18) by macrophages. IFN-I improves TAA retention by dendritic cells and cross-presentation of antigens. Cross-presentation allows dendritic cells to activate CD8+ cytotoxic T-lymphocytes for immune defense against viruses and tumors that do not affect dendritic cells. IFN-I stimulates antibody-dependent cellular cytotoxicity against established liver micrometastases of murine melanoma B16. IFN-I plays a vital role in the development and differentiation of a subset of Th1 T-helper cells that activate macrophages and the generation, activity, expansion, and long-term survival of cytotoxic T-lymphocytes. IFN-I is also responsible for the antitumor activity of NK cells, which prevent tumor growth.
The role of IFN-I in immune metabolism – an interaction between immunological and metabolic processes:
- Signaling following the activation of the pattern recognition receptor (PRR) triggers changes in the metabolism of dendritic cells and macrophages. These changes determine the function of these cells. The cell’s lipid needs are met through a combination of biosynthesis and import programs. After activation of TLR3 in macrophages, IFN-I induced a shift in the balance of lipid metabolism from the cholesterol fatty acids synthesis in favor of the absorption of exogenous lipids. This metabolic shift in macrophages was enough to make the mice resistant to viral infection.
- Stimulation of the TLR9 pattern recognition receptor in plasmacytoid dendritic cells (pDC) led to the autocrine transmission of IFNAR signals (signals acting on the same cell) to increased fatty acid oxidation and oxidative phosphorylation. These reactions are key to the immune functions of the pDC.
- Fasting or introducing calorie restriction mimetics – are supplements that mimic the effect of fasting-improves the effectiveness of immunogenic chemotherapy by depleting regulatory T-cells (Treg) from the tumor microenvironment, which weaken the antitumor immunity. Short-term fasting or treatment with several chemically unrelated calorie restriction mimetics improves anti-cancer immune surveillance and reduces tumor mass. Notably, IFN-I inhibits the proliferation and activity of Treg cells and other immunosuppressive cells, such as myeloid-derived suppressor cells (MDSCs).
Understanding the multi-level interaction between metabolic, immunological, and interferon type I networks will allow for the management of the positive and detrimental immune effects of IFN-I and change the IFN-I-IFNAR axis is therapeutically used during infections and cancer.
The role of type I interferons in antitumor therapy
After discovering interferons, the most significant interest was aroused by the antiviral activity of type I IFN. However, the first U.S. Food and Drug Administration approval for IFN-α2 in 1986 was for cancer treatment.
Even before recombinant IFN was available, several studies conducted on patients with hairy cell leukemia and chronic myelogenous leukemia reported decreased incidence after treatment with partially purified IFN-α. Later, more effective therapeutic regimens than IFN were developed in both cases.
In the following clinical studies, the therapeutic efficacy of IFN-a2 has been reported, either as unmodified recombinant proteins or as pegylated variants. Interferon-alpha-2 contributed to at least partial regression of hematological and solid (with specific localization) tumors, including myelomas, lymphomas, melanomas, Kaposi’s sarcoma, renal cell tumors, and bladder carcinoma.
To date, IFN-α2 is still widely used in combination with interleukin-2 (IL-2) in immunotherapy regimens to treat metastatic renal cell carcinomas and cutaneous melanoma. Currently, more than 100 clinical trials are being conducted worldwide using IFN-α2 as monotherapy or in combination regimens for both hematological and solid malignancies.
Traditional chemotherapy, radiation therapy, and immunotherapy-including oncolytic virotherapy – are particularly effective if they trigger tumor-targeted immune responses. The current view is that therapeutic agents should elicit a combination of stress signals that are usually associated with a viral infection, such as type I IFN signals.
IFN-I is involved in immunogenic cell death, which is a hallmark of successful chemotherapy. Treatment of various types of tumors (fibrosarcoma MCA205 and breast carcinoma AT3) with anthracyclines or oxaliplatin leads to rapid production of IFN-I, mimicking the immune responses caused by viruses. Mechanism of IFN-I-mediated immunogenic cell death:
- Affected dying cancer cells secrete their nucleic acids (especially single-stranded RNAs) into the tumor microenvironment. The TLR3 pattern recognition receptor perceives these nucleic acids on surrounding healthy cells.
- Released type I interferons connect innate and acquired antiviral immunity through a specific ISG signature. It is crucial for the recruitment, selection, and differentiation/maturation of absorbing cells, which determines the immunogenic death of cancer cells.
It is confirmed that the effectiveness of anthracyclines is lost with the co-administration of neutralizing antibodies against IFNAR or IFN-α/β.
In previous studies, IFN-I has been described as a crucial mediator of the non-targeted immunomodulatory effects of cyclophosphamide. This agent triggers the immunogenic death of cancer cells and is responsible for memory expansion of CD4 + and CD8 + T cells, as well as dendritic cells. In patients with hematological malignancies, administration of high doses of cyclophosphamide triggered DNA damage and tumor cell death and led to IFN-I expression. It contributed to establishing a systemic sterile inflammatory response characterized by the release of endogenous signals that can increase the effectiveness of immunotherapy.
Like chemotherapy, radiation therapy increases levels of IFN-I and the protein CXCL10 with antitumor activity in the tumor microenvironment. CXCL10 promotes the destruction of the tumor by CD8+ T cells. IFN-I enhances the antitumor activity of antibodies specific to oncogenic receptors, mobilizing dendritic cells for cross-presentation of TAA to cytotoxic T-lymphocytes.
However, even though these observations strongly confirm the antitumor and immunostimulating effects of IFN-I, the harmful role of interferons in stimulating tumor growth is also reported. As reported above, IFN-I activates PD-L1 in tumor cells, leading to depletion of T cells.
The main goal of research on antitumor immunity remains to identify various molecular networks activated by IFN-I. When and in what ways IFN-I counteracts or promotes tumor growth-this question will be answered in future studies.
Conclusions and prospects
Type I interferons play an essential role in the immune surveillance of cancer and the fight against tumor cells. IFN-I can be produced by both malignant and immune cells and act on them, triggering immune responses by internal and external means of tumor cells.
IFN-I, naturally produced, administered exogenously, or induced by chemotherapy, radiotherapy, or oncolytic virotherapy, have all biological effects through the action of ISG. Attempts to decipher the specific functions of individual ISG in the interaction between cancer and immune cells can help achieve the therapeutic effectiveness of IFN and identify predictive biomarkers of the immune response.
Taking into account the dual role of type I IFN in inhibiting and stimulating tumor growth, it will be essential to understand which subtype of type I IFN, at what point in time, and through what mechanisms loses its anti-cancer effectiveness and begins to suppress the immune system and stimulate the formation of cancer stem cells.
Source
Type-I-interferons in infection and cancer: Unanticipated dynamics with therapeutic implications